Introduction
The digestive process plays a vital role in overall health, and understanding its intricacies is crucial when considering fasting. A comprehensive grasp of stomach digestion and its dynamics is essential for informed decision-making.
Understanding the Importance of Stomach Digestion
Stomach digestion is a critical component of the digestive process, responsible for breaking down food into smaller molecules that can be absorbed and utilized by the body. Effective stomach digestion is essential for maintaining optimal nutrient uptake, preventing digestive disorders, and supporting overall health and well-being. The stomach’s ability to secrete digestive enzymes and acids enables the degradation of proteins, carbohydrates, and fats, facilitating the absorption of vital nutrients. Impaired stomach digestion can lead to a range of complications, including malabsorption, bloating, and abdominal pain. Furthermore, a healthy stomach microbiome plays a crucial role in immune system function, with an imbalance of gut bacteria linked to various diseases. As such, understanding the importance of stomach digestion is vital for promoting healthy eating habits, managing digestive issues, and optimizing overall quality of life.
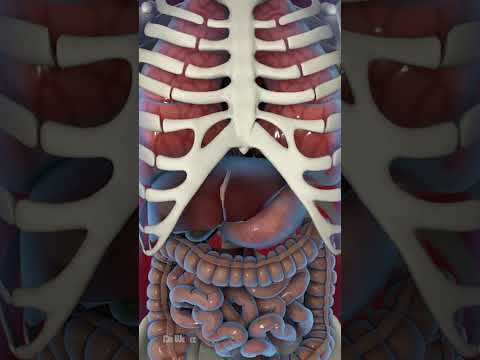
The Digestive System⁚ An Overview
The human digestive system is a complex process involving multiple organs and glands working in concert to break down, absorb, and utilize nutrients from ingested food, spanning the mouth, esophagus, stomach, small intestine, and large intestine.
Key Components of the Digestive System
The digestive system comprises various key components that facilitate the breakdown and absorption of nutrients. The mouth initiates the process through mechanical digestion via mastication, while salivary glands secrete enzymes to commence chemical digestion.
The esophagus acts as a muscular tube, propelling food into the stomach through peristalsis. The stomach, a sac-like organ, secretes digestive enzymes and acids to further degrade ingested matter.
The small intestine, a long, thin tube, is responsible for the majority of nutrient absorption, facilitated by finger-like projections called villi. The large intestine, also known as the colon, absorbs water and electrolytes, while storing and eliminating waste products.
Accessory organs, including the pancreas and liver, contribute to the digestive process by producing enzymes and bile, respectively. A thorough understanding of these key components is essential for comprehending the intricate mechanisms of the digestive system.
Each component plays a vital role in ensuring the efficient breakdown, absorption, and utilization of nutrients, thereby maintaining overall health and well-being.
The Role of Stomach Acid and Digestive Enzymes
Gastric juices, comprising stomach acid and digestive enzymes, play a pivotal role in protein denaturation and nutrient breakdown. Hydrochloric acid (HCl) maintains an acidic pH, activating digestive enzymes and facilitating protein unwinding.
Pepsin, a primary digestive enzyme, breaks down proteins into smaller peptides and amino acids. Additionally, gastric amylase and lipase contribute to carbohydrate and fat digestion, respectively.
Stomach acid also serves as a defense mechanism, sterilizing ingested food and preventing bacterial colonization. Furthermore, it triggers the release of bile salts and pancreatic juices in the small intestine, augmenting the digestive process.
The interplay between stomach acid and digestive enzymes ensures efficient nutrient breakdown and absorption, underscoring the importance of optimal gastric function in maintaining overall health. Any disruptions to this delicate balance can lead to digestive issues and compromise nutritional status.
A comprehensive understanding of the roles of stomach acid and digestive enzymes is essential for appreciating the intricacies of the digestive process.
Fasting Benefits⁚ Separating Fact from Fiction
Fasting has garnered attention for its potential health benefits, but it is crucial to distinguish between evidence-based advantages and unsubstantiated claims, particularly in relation to its impact on digestive health and stomach function.
Debunking Common Misconceptions about Fasting
Several misconceptions surrounding fasting have led to unnecessary concerns and apprehensions. One common myth is that fasting causes muscle loss and decreased metabolism. However, research has shown that intermittent fasting can actually help preserve muscle mass and improve metabolic function.
Another misconception is that fasting leads to nutrient deficiencies. While it is true that fasting involves caloric restriction, a well-planned fasting regimen can ensure adequate nutrient intake. Additionally, fasting has been shown to improve nutrient absorption and utilization.
It is also often believed that fasting is not suitable for everyone, particularly older adults or those with certain health conditions. However, studies have demonstrated that fasting can be beneficial for individuals with various health profiles, including those with type 2 diabetes and cardiovascular disease. By debunking these misconceptions, individuals can make informed decisions about incorporating fasting into their lifestyle.
The Effects of Fasting on Gut Bacteria
Fasting has been shown to have a profound impact on the gut microbiome, leading to changes in the composition and diversity of gut bacteria. During fasting, the gut microbiome undergoes a shift towards a more beneficial profile, with an increase in the production of short-chain fatty acids and antimicrobial peptides.
This shift in the gut microbiome has been linked to improved immune function, reduced inflammation, and enhanced barrier function. Fasting has also been shown to increase the production of certain beneficial gut hormones, such as ghrelin and motilin, which play a crucial role in regulating gut motility and secretion.
Furthermore, studies have demonstrated that fasting can lead to an increase in the abundance of certain beneficial bacterial species, such as Bifidobacterium and Lactobacillus, which are associated with improved gut health and immune function. Overall, the effects of fasting on gut bacteria are complex and multifaceted, and further research is needed to fully understand the mechanisms involved.
The Impact of Fasting on Stomach Digestion
Fasting significantly influences stomach digestion, altering gastric acid secretion, digestive enzyme activity, and gut motility. These changes can have profound effects on nutrient absorption, gut health, and overall digestive well-being.
Fasting Effects on Stomach Acid Production
Fasting has been shown to significantly impact stomach acid production, with studies indicating a decrease in gastric acid secretion during periods of fasting. This reduction in stomach acid can be attributed to several factors, including the decreased stimulation of the parasympathetic nervous system, which regulates digestive processes, and the reduced release of gastrin, a hormone responsible for stimulating gastric acid secretion.
Additionally, fasting has been found to increase the production of certain hormones, such as somatostatin, which can inhibit the release of gastric acid. The decrease in stomach acid production during fasting can have both positive and negative effects on the digestive system, depending on the individual’s specific circumstances. Understanding the effects of fasting on stomach acid production is essential for individuals considering incorporating fasting into their dietary regimen, particularly those with pre-existing digestive issues.
Fasting and Digestive Enzyme Activity
Fasting has been found to influence digestive enzyme activity, with studies indicating changes in the expression and secretion of various enzymes involved in protein, carbohydrate, and fat digestion. During fasting, the pancreas reduces the production of digestive enzymes, such as amylase, lipase, and trypsin, which are normally secreted in response to food intake.
This reduction in digestive enzyme activity can lead to improved efficiency in nutrient absorption and utilization, as the body adapts to the fasting state by increasing the expression of enzymes involved in gluconeogenesis and ketogenesis. Furthermore, fasting has been shown to stimulate the production of certain enzymes involved in cellular cleaning and renewal, such as autophagy-related enzymes. Understanding the effects of fasting on digestive enzyme activity can provide valuable insights into the physiological adaptations that occur during periods of caloric restriction.
A thorough comprehension of these changes can help healthcare professionals develop personalized recommendations for individuals considering fasting as a therapeutic intervention.
Common Stomach Issues When Fasting
Fasting can precipitate various stomach issues, including nausea, vomiting, diarrhea, and abdominal pain, often due to changes in gut motility, acid production, and digestive enzyme activity, warranting careful consideration and management.
Addressing Stomach Problems during Fasting
When stomach problems arise during fasting, it is essential to address them promptly to prevent complications. Patients should seek medical attention if experiencing severe abdominal pain, vomiting blood, or blood in stool. Mild issues, such as nausea and diarrhea, may be managed with hydration, electrolyte supplementation, and over-the-counter medications.
In some cases, adjusting the fasting regimen may be necessary. This may involve altering the duration or frequency of fasts, or incorporating small amounts of easily digestible foods to alleviate symptoms. Probiotics and other supplements may also be recommended to promote gut health and mitigate stomach problems.
A healthcare professional should be consulted for personalized guidance on managing stomach problems during fasting. By working together, patients can develop effective strategies for minimizing discomfort and ensuring a safe and beneficial fasting experience.
Early intervention and proper management are crucial in preventing complications and ensuring the successful completion of the fasting regimen.
Strategies for Mitigating Stomach Issues during Fasting
To minimize stomach issues during fasting, several strategies can be employed. Adequate hydration is essential, and individuals should aim to drink at least eight glasses of water per day. Electrolyte-rich beverages, such as coconut water or sports drinks, can also help maintain electrolyte balance.
Incorporating gentle exercise, such as yoga or walking, can also aid digestion and reduce stomach discomfort. Stress management techniques, including meditation and deep breathing, can help mitigate the negative effects of stress on the digestive system.
Additionally, selecting a fasting schedule that allows for some caloric intake, such as 16⁚8 or 5⁚2, may be beneficial for individuals who experience stomach issues with more restrictive fasting regimens. Probiotics and other supplements may also be considered to promote gut health and alleviate stomach problems.
By incorporating these strategies into their fasting regimen, individuals can reduce the likelihood of stomach issues and ensure a more comfortable and successful fasting experience.
Fasting can have a profound impact on stomach digestion, and understanding its effects is crucial for maintaining optimal gut health. By embracing informed fasting practices, individuals can reap the benefits of fasting while ensuring digestive well-being.
Embracing the Benefits of Fasting for a Healthier Gut
By understanding the complex relationship between fasting and stomach digestion, individuals can harness the benefits of fasting to promote a healthier gut. A well-informed approach to fasting can lead to improved digestive enzyme activity, enhanced gut bacteria diversity, and strengthened stomach lining. Moreover, incorporating fasting into one’s lifestyle can stimulate autophagy, a natural process in which the body breaks down and recycles damaged cells and proteins, leading to cellular renewal and rejuvenation. As research continues to uncover the intricacies of fasting’s impact on gut health, it is essential to consult with healthcare professionals to determine the most suitable fasting regimen for individual needs. By embracing the benefits of fasting, individuals can take a proactive step towards cultivating a balanced and resilient gut microbiome, ultimately contributing to overall well-being and quality of life.
This article provides a thorough introduction to the importance of stomach digestion and its role in overall health. The writing is clear and concise, making it accessible to readers without prior knowledge of human physiology.
As someone who has struggled with digestive issues in the past, I found this article incredibly informative and reassuring. The explanation of impaired stomach digestion
I appreciated how this article touched upon lesser-known aspects of stomach health like gut bacteria
While I found this article engaging overall, I felt that certain sections – such as “The Digestive System⁚ An Overview” – were somewhat dry due to their technical nature.
This article effectively conveys complex information about human physiology without becoming overwhelming or jargon-heavy – no easy feat! Nonetheless some illustrations or diagrams would enhance reader comprehension.
I appreciate how this article highlights the interconnectedness of the digestive system