What are Antipsychotic Drugs?
Antipsychotic drugs are psychiatric medications primarily used to manage psychosis, including hallucinations and delusions, in conditions such as schizophrenia and bipolar disorder, playing a crucial role in mental health treatment.
Definition and Purpose
Antipsychotic drugs are a class of psychiatric medications designed to alleviate symptoms of psychosis, which include hallucinations, delusions, and disorganized thinking. The primary purpose of antipsychotics is to manage and control these symptoms in individuals diagnosed with various mental health conditions, such as schizophrenia, bipolar disorder, and severe depression with psychotic features.
The ultimate goal of antipsychotic treatment is to improve the quality of life for affected individuals, enabling them to function more effectively in their daily lives. By mitigating the severity of psychotic symptoms, antipsychotics can help restore a sense of reality, reduce anxiety and agitation, and promote a more stable mental state. As a fundamental component of comprehensive mental health treatment, antipsychotic medications play a vital role in facilitating recovery and rehabilitation for individuals struggling with psychotic disorders.
Through their targeted mechanisms of action, antipsychotics serve as a crucial therapeutic tool, helping to alleviate the distressing symptoms of psychosis and improve overall mental health outcomes.
Common Conditions Treated with Antipsychotics
Antipsychotic medications are commonly used to treat a range of mental health conditions characterized by psychotic symptoms, including schizophrenia, bipolar disorder, and severe depression with psychotic features.
Schizophrenia is a chronic condition marked by hallucinations, delusions, and disorganized thinking, and antipsychotics are often the first line of treatment. Bipolar disorder, which involves episodes of mania or hypomania, may also be treated with antipsychotics, particularly during acute episodes.
In addition, antipsychotics may be prescribed for individuals with severe depression who experience psychotic symptoms, such as hallucinations or delusions. Other conditions that may be treated with antipsychotics include schizoaffective disorder, brief psychotic disorder, and substance-induced psychosis. By effectively managing psychotic symptoms, antipsychotics can significantly improve the quality of life for individuals affected by these conditions.
It is essential to note that antipsychotics are typically used in conjunction with other treatments, such as psychotherapy and lifestyle modifications, to achieve optimal outcomes.
How Do Antipsychotics Work?
Antipsychotics work by modulating neurotransmitter activity in the brain, primarily functioning as dopamine blockers, serotonin antagonists, and mood stabilizers to alleviate psychotic symptoms and restore balanced mental functioning.
Blocking Dopamine Receptors
The primary mechanism of action of antipsychotics involves blocking dopamine receptors in the brain, specifically D2 receptors. This blockade helps to reduce the excessive dopamine activity that is thought to contribute to the development of psychotic symptoms, such as hallucinations and delusions. By inhibiting dopamine’s action, antipsychotics can alleviate these symptoms and restore more balanced neurotransmitter activity.
Dopamine receptor blockade is also associated with the therapeutic effects of antipsychotics on mood stabilization and cognitive function. The specific affinity of antipsychotics for D2 receptors can vary, influencing their efficacy and side effect profiles. Overall, the dopamine-blocking action of antipsychotics is a crucial component of their therapeutic mechanism, allowing for effective management of psychosis and related symptoms in various psychiatric conditions.
This pharmacological action has significant implications for our understanding of the neurochemical basis of psychosis and the development of novel therapeutic strategies for its treatment.
Serotonin Antagonism
In addition to dopamine receptor blockade, many antipsychotics also exhibit serotonin antagonism, which contributes to their therapeutic effects. Serotonin receptors, particularly 5-HT2A receptors, are involved in the regulation of mood, cognition, and perception. By blocking these receptors, antipsychotics can mitigate symptoms such as anxiety, agitation, and depression.
Serotonin antagonism is thought to be particularly important in the treatment of negative symptoms, such as apathy and social withdrawal, which are often observed in schizophrenia. Furthermore, serotonin receptor blockade may help to reduce the risk of extrapyramidal side effects associated with dopamine receptor blockade. The balance between dopamine and serotonin receptor antagonism can influence the efficacy and tolerability of antipsychotics, highlighting the complexity of their pharmacological mechanisms.
The interplay between dopamine and serotonin systems is an active area of research, with ongoing efforts to optimize antipsychotic treatment strategies by targeting these neurotransmitter systems.
Mood Stabilization
Beyond their antipsychotic effects, many of these medications also exhibit mood-stabilizing properties, which can be beneficial in the treatment of mood disorders such as bipolar disorder. Mood stabilization is thought to occur through a combination of mechanisms, including modulation of neurotransmitter systems and neuroplasticity.
Some antipsychotics have been shown to decrease the excitability of neurons, leading to a reduction in the extreme mood swings characteristic of bipolar disorder. Additionally, antipsychotics may influence the expression of genes involved in mood regulation, contributing to their mood-stabilizing effects.
The mood-stabilizing properties of antipsychotics can be particularly useful in the treatment of patients with co-occurring psychotic and mood symptoms. By addressing both symptom domains, antipsychotics can help to improve overall treatment outcomes and quality of life for individuals with complex psychiatric conditions.
Types of Antipsychotics
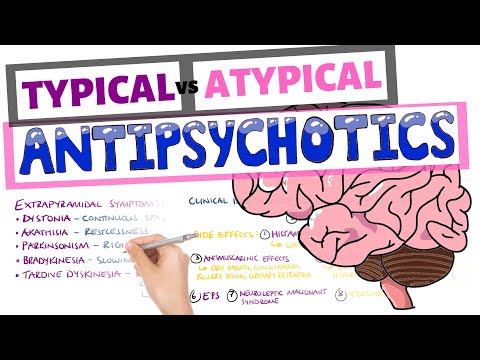
Antipsychotic medications can be broadly classified into distinct categories, primarily first-generation and second-generation antipsychotics, each with unique pharmacological profiles, therapeutic effects, and side effect liabilities in psychiatric treatment.
First-Generation Antipsychotics
First-generation antipsychotics, also known as typical antipsychotics, primarily function as dopamine blockers, thereby alleviating symptoms of psychosis in individuals with schizophrenia and other related disorders. These medications, introduced in the 1950s, were the first effective treatments for psychosis and revolutionized psychiatric care.
Examples of first-generation antipsychotics include chlorpromazine, haloperidol, and fluphenazine. While these medications are effective in managing hallucinations and delusions, they often cause extrapyramidal side effects, such as tremors, rigidity, and bradykinesia. Additionally, they may lead to tardive dyskinesia, a potentially irreversible movement disorder.
Due to the risk of these adverse effects, first-generation antipsychotics are generally reserved for treating patients who have not responded to second-generation antipsychotics or have specific clinical indications. However, they remain an essential component of the antipsychotic pharmacopeia, providing a valuable treatment option for selected individuals with severe mental illness.
Second-Generation Antipsychotics
Second-generation antipsychotics, also known as atypical antipsychotics, were introduced in the 1990s and have since become the preferred treatment for psychosis due to their improved side effect profile compared to first-generation antipsychotics.
Examples of second-generation antipsychotics include risperidone, olanzapine, quetiapine, and aripiprazole. These medications combine dopamine blockade with serotonin antagonism, which is thought to contribute to their reduced risk of extrapyramidal side effects. Additionally, they may offer benefits in terms of mood stabilization and reduced risk of tardive dyskinesia.
Second-generation antipsychotics are commonly used to treat a range of conditions, including schizophrenia, bipolar disorder, and major depressive disorder with psychotic features. While they are generally better tolerated than first-generation antipsychotics, they can still cause significant side effects, such as weight gain, metabolic changes, and sedation. As with any medication, careful consideration of the potential benefits and risks is essential when prescribing second-generation antipsychotics.
Benefits and Risks of Antipsychotics
Antipsychotic medications offer significant benefits in managing psychosis, improving quality of life, and reducing symptoms of schizophrenia and bipolar disorder, but also carry risks of adverse effects and require careful monitoring.
Efficacy in Treating Psychosis
Antipsychotic medications have demonstrated efficacy in treating psychosis, particularly in reducing the severity of hallucinations and delusions. Studies have consistently shown that antipsychotics can significantly improve symptoms of schizophrenia and bipolar disorder, enhancing overall quality of life for individuals affected by these conditions.
Clinical trials have also highlighted the importance of early intervention with antipsychotics, as prompt treatment initiation can lead to better outcomes and improved treatment response. Furthermore, antipsychotics have been found to be effective in both acute and maintenance phases of treatment, providing sustained symptom relief and reducing the risk of relapse.
The efficacy of antipsychotics is thought to be attributed to their ability to modulate neurotransmitter systems, primarily dopamine and serotonin, which play a crucial role in the development of psychotic symptoms. By targeting these systems, antipsychotics can help restore balance and alleviate the distressing symptoms of psychosis.
Potential Side Effects
Antipsychotic medications, like all psychiatric medications, can cause a range of potential side effects. Common adverse effects include weight gain, sedation, and extrapyramidal symptoms (EPS) such as tremors and rigidity. Additionally, some antipsychotics may increase the risk of metabolic disorders, including diabetes and dyslipidemia.
Other possible side effects of antipsychotics include orthostatic hypotension, anticholinergic effects, and hyperprolactinemia. In rare cases, antipsychotics may also be associated with more severe side effects, such as neuroleptic malignant syndrome (NMS) and tardive dyskinesia. It is essential to carefully monitor patients for these potential side effects and to adjust treatment as needed to minimize their occurrence and impact.
A thorough discussion of the potential risks and benefits of antipsychotic treatment should be conducted with each patient, taking into account their individual needs and health status. This informed approach can help optimize treatment outcomes while minimizing the risk of adverse effects.
Monitoring and Maintenance
To ensure optimal treatment outcomes with antipsychotic medications, regular monitoring and maintenance are essential. This includes frequent assessments of the patient’s mental health status, as well as monitoring for potential side effects.
A comprehensive treatment plan should involve a multidisciplinary approach, incorporating input from psychiatrists, primary care physicians, and other healthcare professionals as needed. Regular follow-up appointments should be scheduled to assess treatment efficacy, adjust medication regimens as necessary, and provide ongoing support and education to patients and their families.
By maintaining a collaborative and patient-centered approach, clinicians can help optimize treatment adherence, minimize the risk of relapse, and improve overall quality of life for individuals receiving antipsychotic treatment. Effective monitoring and maintenance are critical to achieving long-term success in managing psychosis and related conditions with antipsychotic medications.
Current Research and Future Directions
Ongoing research focuses on developing novel antipsychotic agents with improved efficacy and tolerability, as well as exploring innovative treatment strategies, including personalized medicine and adjunctive therapies, to enhance mental health outcomes.
New Developments in Antipsychotic Medications
Recent advancements in antipsychotic medications have led to the development of novel compounds with distinct pharmacological profiles. These new agents aim to address the limitations of existing treatments, such as inadequate efficacy, poor tolerability, and significant side effects. Researchers are exploring various strategies, including the development of dopamine-sparing antipsychotics, which may reduce the risk of extrapyramidal symptoms and tardive dyskinesia. Additionally, several investigational agents targeting glutamatergic and GABAergic systems are being evaluated for their potential to improve cognitive function and alleviate negative symptoms in patients with schizophrenia. Furthermore, advancements in pharmacogenomics and precision medicine may enable personalized treatment approaches, allowing clinicians to tailor antipsychotic therapy to an individual’s unique genetic profile and medical needs.
Personalized Treatment Approaches
The integration of pharmacogenomics, neuroimaging, and clinical data is enabling the development of personalized treatment approaches for patients with psychotic disorders. By analyzing an individual’s genetic profile, clinicians can identify potential genetic variants that may influence their response to antipsychotic medications. This information can be used to guide treatment decisions, optimizing the selection of medication and dosage to minimize adverse effects and maximize therapeutic efficacy. Furthermore, the use of neuroimaging techniques, such as functional magnetic resonance imaging (fMRI), can provide valuable insights into brain function and structure, allowing clinicians to tailor treatment to specific neural circuitry abnormalities. Ultimately, personalized treatment approaches aim to improve treatment outcomes, reduce healthcare costs, and enhance the overall quality of life for patients with psychotic disorders.
Integration with Other Mental Health Treatments
The effective management of psychotic disorders often requires the integration of antipsychotic medications with other mental health treatments. Psychotherapy, such as cognitive-behavioral therapy (CBT) and family therapy, can be a valuable adjunct to pharmacological interventions, helping patients to develop coping strategies, manage symptoms, and improve relationships. Additionally, social support services, including case management and vocational rehabilitation, can facilitate recovery by addressing practical needs and promoting social inclusion. Furthermore, the incorporation of lifestyle modifications, such as regular exercise and healthy eating, can also contribute to overall well-being. A multidisciplinary approach, combining the expertise of psychiatrists, psychologists, social workers, and other healthcare professionals, is essential for providing comprehensive care and optimizing treatment outcomes for individuals with psychotic disorders. By integrating antipsychotic medications with other mental health treatments, clinicians can provide patient-centered care that addresses the complex needs of this population.
Overall this is an informative piece that effectively conveys complex information about antipsychotics One minor suggestion would be incorporating case studies examples illustrating successful application treatments aid comprehension among non-experts.
This article serves as a useful resource for understanding the fundamentals of antipsychotic drugs. Nevertheless, I believe it would benefit from additional information on non-pharmacological interventions that can complement antipsychotic treatment.
The writing style is clear and concise throughout the article making it accessible to readers without extensive medical backgrounds I particularly appreciated how it emphasizes restoring reality reducing anxiety agitation promoting stability through targeted medication
This article provides an excellent overview of antipsychotic drugs and their role in managing psychosis in various mental health conditions. The definition and purpose section effectively explains the primary objectives of antipsychotic treatment.
The section on common conditions treated with antipsychotics provides valuable insights into the specific applications of these medications. I would like to see further discussion on emerging trends in antipsychotic research and development.
I appreciate how this article highlights the importance of antipsychotics in improving the quality of life for individuals with psychotic disorders. However, it would be beneficial to include more information on potential side effects associated with these medications.