Introduction
Chronic wounds pose significant challenges for healthcare systems and patients worldwide. Slow healing wounds, in particular, necessitate comprehensive care to prevent prolonged recovery, mitigate risks of complications, and improve patient outcomes and quality of life.
What are Slow Healing Wounds?
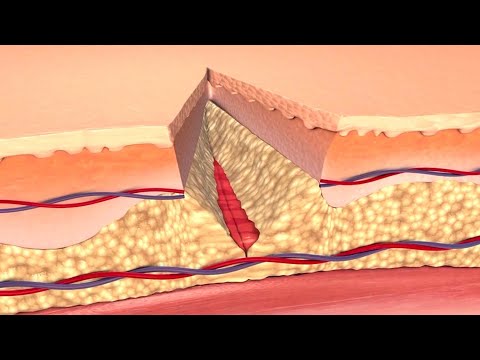
Slow healing wounds, also known as chronic wounds, are lesions that fail to progress through the normal stages of healing, remaining in a state of arrested development for an extended period. This phenomenon occurs when the complex interplay of cellular, biochemical, and molecular processes that govern wound repair is disrupted.
Characterized by a persistent defect in the skin or underlying tissues, slow healing wounds can arise from various etiologies, including traumatic injury, surgical intervention, or as a consequence of underlying disease. The protracted nature of these wounds leads to increased susceptibility to infection, inflammation, and tissue damage, further complicating the healing process.
The burden of slow healing wounds on healthcare systems and individual patients is substantial, necessitating sustained clinical attention and resource allocation to manage symptoms, promote healing, and minimize the risk of long-term disability and morbidity. Effective management of these challenging wounds requires a multidisciplinary approach, integrating the expertise of healthcare professionals from diverse specialties to address the complex needs of affected patients.
Definition and Types
Slow healing wounds encompass various clinical entities, including skin ulcers, pressure sores, diabetic foot ulcers, and venous leg ulcers. These lesions are characterized by delayed or absent healing, often resulting in prolonged morbidity and disability.
Causes and Risk Factors
Slow healing wounds are often the result of a complex interplay between intrinsic and extrinsic factors. Intrinsic factors include patient-related variables such as age, nutrition, and overall health status. Extrinsic factors, on the other hand, comprise environmental and iatrogenic elements, including wound trauma, infection, and inadequate wound care.
Certain medical conditions, such as diabetes mellitus, arterial insufficiency, and venous hypertension, can also significantly impede the healing process. Additionally, medications like corticosteroids and anticoagulants may negatively impact wound recovery by altering the body’s natural response to injury.
Moreover, lifestyle factors such as smoking, physical inactivity, and poor nutrition can contribute to delayed wound healing. A comprehensive understanding of these causes and risk factors is essential for the development of effective prevention and treatment strategies for slow healing wounds. By identifying and addressing these underlying factors, healthcare professionals can optimize wound care and improve patient outcomes. Early recognition and management of these risk factors are critical in preventing prolonged recovery and mitigating the risk of complications.
Underlying Medical Conditions
Certain underlying medical conditions can significantly impede the healing process of wounds. Diabetes mellitus, for instance, is a major risk factor for slow healing wounds due to its associated neuropathy, peripheral arterial disease, and impaired immune function.
Vascular diseases, such as arterial insufficiency and venous hypertension, can also compromise wound healing by reducing blood flow and oxygen delivery to the affected tissue. Additionally, conditions like rheumatoid arthritis, lupus, and scleroderma can lead to chronic inflammation, which can further hinder the healing process.
Neurological disorders, such as spinal cord injuries and multiple sclerosis, can also increase the risk of slow healing wounds due to impaired sensory perception and motor function. Furthermore, gastrointestinal disorders, like Crohn’s disease and ulcerative colitis, can lead to malabsorption of essential nutrients, which are critical for wound recovery. Understanding the impact of these underlying medical conditions on wound healing is crucial for developing effective treatment strategies and optimizing patient outcomes.
By recognizing and managing these conditions, healthcare professionals can mitigate their negative effects on wound healing and promote a more efficient recovery process.
External Factors
External factors, including pressure, friction, and shear forces, can significantly impede wound healing. Additionally, exposure to environmental stressors, such as extreme temperatures and humidity, can also compromise the recovery process of slow healing wounds.
Consequences of Slow Healing Wounds
Slow healing wounds can have far-reaching and devastating consequences for individuals, affecting not only their physical health but also their emotional and social well-being. The prolonged recovery process can lead to increased healthcare costs, extended hospital stays, and a significant economic burden on patients and their families.
Furthermore, slow healing wounds can result in persistent pain, discomfort, and limited mobility, thereby compromising an individual’s ability to engage in daily activities and maintain independence. The emotional toll of coping with a chronic wound can be substantial, leading to feelings of frustration, anxiety, and depression.
The consequences of slow healing wounds can also extend beyond the individual, impacting healthcare systems and society as a whole. The increased demand for wound care services and resources can place a significant strain on healthcare systems, highlighting the need for effective prevention and management strategies to mitigate the consequences of slow healing wounds.
Physical and Emotional Impact
The physical impact of slow healing wounds can be profound, leading to chronic pain, discomfort, and limited mobility. Patients may experience sleep disturbances, fatigue, and decreased appetite, which can further compromise the healing process. Additionally, prolonged immobility can result in muscle atrophy, joint contractures, and decreased range of motion.
The emotional toll of coping with a slow healing wound should not be underestimated. Patients often experience feelings of frustration, anxiety, and depression, which can be exacerbated by the loss of independence and autonomy. Social isolation and decreased participation in activities of daily living can also contribute to a decline in mental health and well-being.
Moreover, the physical and emotional impact of slow healing wounds can be interrelated, creating a vicious cycle of decreased mobility, increased pain, and compromised mental health. Effective wound management strategies must therefore address both the physical and emotional needs of patients to promote optimal outcomes and improve quality of life.
Increased Risk of Complications
Slow healing wounds are susceptible to infection, sepsis, and osteomyelitis, which can lead to prolonged hospitalization, increased morbidity, and mortality. Delayed healing also increases the risk of wound progression, necessitating more extensive and complex treatments.
Wound Management and Treatment Strategies
Effective wound management is crucial to prevent prolonged healing, reduce the risk of complications, and improve patient outcomes. A multidisciplinary approach is often necessary, involving healthcare professionals from various specialties.
A comprehensive treatment plan should be tailored to the individual’s specific needs, taking into account the underlying cause of the wound, as well as any comorbidities or external factors that may be impacting healing.
This may involve a combination of conventional therapies, such as wound cleansing, debridement, and dressing changes, as well as advanced treatments, including topical growth factors, skin substitutes, and negative pressure wound therapy.
Regular monitoring and reassessment of the wound are essential to ensure that the treatment plan is effective and to make any necessary adjustments. By adopting a holistic and patient-centered approach to wound care, healthcare professionals can optimize healing outcomes and improve the overall quality of life for individuals with slow healing wounds.
Early intervention and ongoing support are critical components of successful wound management, enabling individuals to regain independence and mobility, and reducing the economic burden associated with prolonged wound care.
Comprehensive Wound Care
A comprehensive wound care plan is essential for promoting healing, preventing complications, and improving patient outcomes. This approach involves a thorough assessment of the individual’s overall health, including any underlying medical conditions, nutritional status, and lifestyle factors.
The wound itself is also carefully evaluated, including its size, depth, and location, as well as the presence of any signs of infection or tissue damage. Based on these findings, a personalized treatment plan is developed, incorporating evidence-based therapies and interventions.
This may include wound cleansing and debridement, dressing changes, and topical treatments, such as antimicrobial agents or growth factors. Pain management is also a critical component of comprehensive wound care, as uncontrolled pain can significantly impair healing and quality of life.
Ongoing education and support are provided to empower individuals to take an active role in their wound care, including guidance on proper wound maintenance, nutrition, and lifestyle modifications; By adopting a comprehensive and patient-centered approach, healthcare professionals can optimize wound healing outcomes and improve overall patient well-being.
Regular monitoring and reassessment of the wound are also crucial to ensure that the treatment plan is effective and to make any necessary adjustments.
Advanced Therapies
Negative pressure wound therapy, hyperbaric oxygen therapy, and bioengineered skin substitutes are advanced treatment options for slow healing wounds, promoting tissue regeneration, reducing bacterial loads, and enhancing wound closure rates in complex cases.
In conclusion, effective management of slow healing wounds requires a multidisciplinary approach, integrating comprehensive wound care and advanced therapies to address the complex needs of patients.
It is crucial for healthcare professionals to stay updated on the latest evidence-based practices and technologies to provide high-quality care and improve patient outcomes.
Furthermore, awareness and education on wound prevention and management should be promoted among patients, caregivers, and the general public to reduce the incidence of slow healing wounds and alleviate their physical and emotional impact.
By adopting a proactive and holistic approach to wound care, individuals can minimize the risk of complications and optimize their chances of recovery, thereby enhancing their overall quality of life.
Ultimately, a concerted effort from healthcare providers, policymakers, and the community is necessary to address the challenges posed by slow healing wounds and ensure that patients receive the best possible care.
Early Intervention and Prevention
Early intervention and prevention are critical components in managing slow healing wounds. Identifying high-risk patients and implementing preventive measures can significantly reduce the incidence of chronic wounds.
Regular assessment and monitoring of patients with underlying medical conditions, such as diabetes or venous insufficiency, can facilitate timely interventions and prevent wound development.
Patient education on proper wound care, skincare, and footwear selection is also essential in preventing wounds and promoting healing.
In addition, healthcare providers should encourage patients to adopt healthy lifestyle habits, such as regular exercise, balanced diet, and smoking cessation, to promote overall health and well-being.
By prioritizing early intervention and prevention, healthcare providers can mitigate the physical and emotional impact of slow healing wounds, reduce healthcare costs, and improve patient outcomes.
A proactive approach to wound care can also facilitate early detection of potential complications, enabling prompt treatment and minimizing the risk of adverse consequences.
I appreciate how this article emphasizes the importance of a multidisciplinary approach in managing slow healing wounds. As a nurse practitioner specializing in wound care, I can attest that collaboration among healthcare professionals is crucial in promoting optimal patient outcomes.
Overall; this article serves as an excellent primer for healthcare professionals seeking to enhance their understanding of slow healing wounds; its clarity; organization; make it an enjoyable read.
While this article provides an excellent introduction to slow healing wounds, I would have liked to see more discussion on evidence-based treatment strategies for specific types of chronic wounds. Future articles could delve deeper into best practices for wound management.
The section on causes and risk factors was particularly informative; however; I felt that it could have been expanded upon further to include more details about how comorbidities contribute to impaired wound healing.
This article provides a comprehensive overview of slow healing wounds, highlighting their definition, types, causes, and risk factors. The language used is clear and concise, making it accessible to healthcare professionals across various disciplines.