Achilles Tendon Rupture⁚ A Comprehensive Overview
Achilles tendon rupture is a severe musculoskeletal injury involving sudden, complete, or partial disruption of the Achilles tendon, necessitating prompt medical attention to prevent long-term disability and optimize functional recovery.
Introduction
Achilles tendon rupture is a debilitating injury that affects individuals across various age groups and activity levels. It is particularly prevalent among athletes participating in high-impact sports, such as football, basketball, and tennis. The Achilles tendon, being the thickest and strongest tendon in the human body, plays a crucial role in facilitating movement, stability, and propulsion. Despite its remarkable tensile strength, the Achilles tendon remains susceptible to acute and chronic injuries, with rupture being the most severe and clinically significant. The consequences of an Achilles tendon rupture can be far-reaching, resulting in prolonged periods of immobilization, rehabilitation, and potentially permanent functional impairment. Therefore, a comprehensive understanding of the underlying causes, clinical presentation, diagnostic modalities, and therapeutic options is essential for optimizing patient outcomes and minimizing long-term morbidity.
Anatomy and Causes
The Achilles tendon’s complex anatomy and multifactorial causes contribute to its susceptibility to rupture, involving intrinsic tendon degeneration, extrinsic biomechanical factors, and systemic influences that compromise its structural integrity.
Anatomical Considerations
The Achilles tendon is a complex, dynamic structure composed of type I collagen fibers, elastin, and proteoglycans. It originates from the myotendinous junctions of the gastrocnemius and soleus muscles, converging to form a thick, fibrous cord that inserts onto the calcaneal tuberosity. The tendon’s unique anatomy, featuring a twist in its mid-portion, creates an area of high stress concentration. A surrounding paratenon, richly innervated with nociceptors and mechanoreceptors, provides proprioceptive feedback and facilitates smooth tendon gliding. The Achilles tendon’s blood supply, derived from the peroneal and posterior tibial arteries, is limited, particularly in its mid-portion, rendering it susceptible to ischemic degeneration. Understanding these anatomical features is crucial for appreciating the pathophysiology of Achilles tendon rupture and developing effective prevention and treatment strategies.
Causes and Risk Factors
Achilles tendon rupture is typically precipitated by a combination of intrinsic and extrinsic factors. Intrinsic risk factors include advanced age, male sex, obesity, and pre-existing tendon degeneration. Individuals with a history of Achilles tendinopathy, rheumatological conditions, or gait disturbances are also at increased risk. Extrinsic factors, such as sudden changes in physical activity, inadequate warm-up or cool-down exercises, and poor footwear, can contribute to tendon rupture. Furthermore, participation in high-impact sports, such as tennis, basketball, or soccer, increases the likelihood of Achilles tendon rupture. The use of corticosteroids and certain antibiotics has also been linked to an elevated risk of tendon rupture. Identifying these causes and risk factors is essential for developing targeted prevention strategies and mitigating the incidence of this debilitating injury.
Symptoms and Diagnosis
Achilles tendon rupture presents with sudden, severe pain and impaired ankle function, necessitating a prompt and accurate diagnostic evaluation to confirm the extent of injury and guide subsequent management decisions.
Clinical Presentation
Achilles tendon rupture typically presents with a sudden, severe pain in the posterior aspect of the ankle, often accompanied by an audible snap or pop. The patient may report feeling as if they have been struck from behind. Swelling and bruising in the affected area are common, with impaired ankle function and difficulty weight-bearing on the affected limb. A palpable defect in the tendon may be evident on physical examination, and the patient may exhibit a positive Thompson test, where compression of the calf muscles fails to produce the normal plantar flexion response. The clinical presentation may vary depending on the severity of the injury, with partial ruptures potentially presenting with less dramatic symptoms. A comprehensive clinical evaluation is essential to accurately diagnose Achilles tendon rupture and guide subsequent management decisions.
Diagnostic Modalities
Diagnosis of Achilles tendon rupture is primarily clinical, but imaging modalities can provide valuable confirmation and assess the extent of the injury. Plain radiographs may be used to rule out associated bony injuries, while ultrasound evaluation can provide a dynamic assessment of the tendon’s integrity. Magnetic Resonance Imaging (MRI) is the modality of choice for evaluating Achilles tendon ruptures, offering high sensitivity and specificity in detecting full or partial tears, as well as assessing the degree of tendon retraction and any associated soft tissue injuries. Computed Tomography (CT) scans may also be employed in certain cases, particularly if there are concerns regarding bony involvement or calcification within the tendon. A diagnostic algorithm incorporating clinical examination and imaging findings enables accurate diagnosis and facilitates informed decision-making regarding treatment options.
Treatment Options
Treatment of Achilles tendon rupture can be broadly categorized into non-surgical and surgical modalities, with the optimal approach determined by patient-specific factors, including activity level, age, and overall health status.
Non-Surgical Management
Non-surgical management of Achilles tendon rupture is typically reserved for patients who are less active, elderly, or possess significant medical comorbidities that preclude surgical intervention. This approach entails a prolonged period of immobilization, often utilizing a plaster cast or removable orthotic device, to facilitate tendon healing.
A graduated rehabilitation program is subsequently implemented to promote progressive strengthening and mobilization of the affected lower limb. Key components of this program include pain management, ankle range-of-motion exercises, and calf strengthening protocols.
While non-surgical management can yield satisfactory outcomes in select patients, it is essential to acknowledge that this approach is associated with a higher risk of rerupture and functional impairment compared to surgical intervention. Therefore, careful patient selection and close clinical monitoring are crucial to optimize treatment success.
Clinical follow-up is necessary to assess the efficacy of non-surgical management and to determine if an alternative treatment strategy may be warranted.
Surgical Intervention
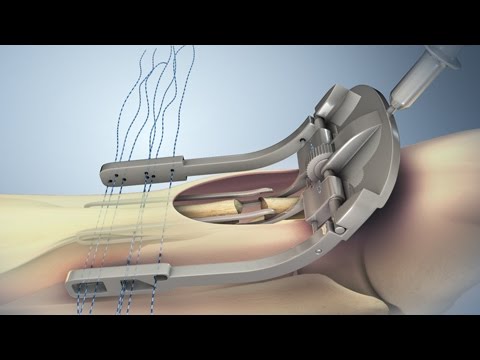
Surgical intervention is a commonly employed treatment modality for Achilles tendon rupture, particularly in young and active individuals. The primary objective of surgery is to restore tendon continuity, promote optimal healing, and minimize the risk of rerupture.
Open or percutaneous surgical techniques may be utilized, with the choice of approach often dictated by surgeon preference and patient-specific factors. The procedure typically involves reapproximation of the tendon ends, followed by secure fixation using sutures, staples, or other specialized devices.
Surgical intervention offers several advantages, including reduced risk of rerupture, improved functional outcomes, and enhanced patient satisfaction. Furthermore, surgical management enables early mobilization and rehabilitation, which can expedite the recovery process and facilitate a timely return to athletic or occupational activities.
A well-executed surgical plan, combined with careful postoperative management, is crucial to achieving optimal outcomes and minimizing complications in patients undergoing surgical repair of Achilles tendon rupture.
Post-Operative Rehabilitation
A well-structured post-operative rehabilitation program is essential to optimize recovery and functional outcomes following surgical repair of Achilles tendon rupture. The primary objectives of rehabilitation are to restore tendon strength, promote healing, and facilitate a safe return to athletic or occupational activities.
The rehabilitation protocol typically commences with a period of immobilization, followed by progressive mobilization and strengthening exercises. A graduated program of weight-bearing, range-of-motion, and resistance exercises is implemented to enhance tendon strength and promote proprioception.
Throughout the rehabilitation process, regular clinical assessments and imaging studies may be performed to monitor tendon healing and adjust the treatment plan as necessary. It is crucial to avoid premature return to high-level activities, as this can increase the risk of rerupture or other complications. By adhering to a carefully designed rehabilitation protocol, patients can achieve optimal outcomes and minimize the risk of long-term disability.
Early rehabilitation typically lasts 6-12 weeks.
Complications and Outcomes
Achilles tendon rupture can result in significant short-term and long-term complications, with treatment outcomes influenced by factors including rupture severity, patient age, and rehabilitation protocol adherence and effectiveness.
Potential Complications
Achilles tendon rupture can lead to various complications, including wound infection, nerve damage, and rerupture. Adhesions and scar tissue formation may also occur, potentially affecting ankle range of motion and function.
Venous thromboembolism is a concern due to prolonged immobilization, emphasizing the need for early mobilization and anticoagulation prophylaxis in high-risk patients. Furthermore, tendon elongation, calf atrophy, and decreased muscle strength may result from inadequate or incomplete rehabilitation.
Additionally, patients may experience chronic pain, swelling, or residual weakness, impacting quality of life and return to preinjury activity levels. The risk of these complications underscores the importance of prompt, specialized treatment and careful postoperative management to minimize morbidity and optimize outcomes following Achilles tendon rupture.
Early recognition and management of potential complications are critical to preventing long-term sequelae and ensuring successful recovery and rehabilitation.
Long-Term Outcomes
Research indicates that patients with Achilles tendon rupture can achieve satisfactory long-term outcomes with appropriate treatment and rehabilitation. Functional recovery is typically evaluated through standardized assessments, such as the Achilles Tendon Rupture Score (ATRS).
Most patients can expect to regain near-normal strength, ankle range of motion, and functional ability within 12-18 months postinjury. However, minor residual deficits may persist, particularly in athletes or individuals with high physical demands.
Factors influencing long-term outcomes include age, preinjury activity level, rupture severity, and rehabilitation quality. A well-structured rehabilitation program emphasizing early mobilization, progressive strengthening, and plyometric training is essential for optimal recovery.
Ultimately, successful long-term outcomes depend on a combination of timely medical intervention, careful postoperative management, and patient commitment to rehabilitation. With proper care, most individuals can recover from Achilles tendon rupture and return to their desired activities with minimal lasting impairment.
Prevention Strategies
Implementing evidence-based prevention strategies, including eccentric strengthening exercises, plyometric training, and gradual progression of athletic activities, can significantly reduce the risk of Achilles tendon rupture in high-risk populations and athletes.
Injury Prevention
Injury prevention is a critical component of Achilles tendon rupture management. A well-structured training program that incorporates strengthening exercises, flexibility drills, and plyometric activities can help mitigate the risk of injury. Specifically, eccentric strengthening exercises targeting the gastrocnemius and soleus muscles have been shown to be effective in reducing the incidence of Achilles tendon ruptures. Additionally, incorporating agility and speed drills into athletic training programs can improve neuromuscular control and reduce the likelihood of injury. It is also essential to address biomechanical abnormalities, such as foot pronation or supination, through the use of orthotics or shoe modifications. Furthermore, adequate warm-up and cool-down periods, as well as regular stretching exercises, can help reduce muscle-tendon stress and prevent injuries. By implementing these evidence-based strategies, individuals can significantly reduce their risk of sustaining an Achilles tendon rupture.
The section on anatomy and causes provides valuable insights into the complex factors contributing to Achilles tendon rupture. However, it would benefit from additional illustrations or diagrams to facilitate understanding.
I was impressed by the article
This article provides an excellent overview of Achilles tendon rupture. The introduction effectively sets the stage for the importance of prompt medical attention to prevent long-term disability.
This article highlights the importance of early diagnosis and treatment for optimal patient outcomes following an Achilles tendon rupture. I appreciate the emphasis on minimizing long-term morbidity.
As an orthopedic surgeon, I found this article to be informative and well-researched. However, I would have liked more discussion on surgical treatment options for Achilles tendon rupture.
I appreciate how the article highlights the prevalence of Achilles tendon rupture among athletes participating in high-impact sports. This emphasizes the need for preventive measures in these populations.
As a physical therapist specializing in sports medicine rehabilitation programs could benefit from more detailed information on post-injury rehabilitation protocols.