Introduction
Adult acne is a prevalent skin condition affecting millions worldwide․ Despite its commonality, the causes of adult acne remain poorly understood․ This article aims to elucidate the underlying factors contributing to adult acne development․
Causes of Adult Acne
Adult acne is a multifactorial disorder, resulting from the interplay of various etiological factors․ The pathogenesis of adult acne involves a complex array of variables, including intrinsic and extrinsic elements․ Intrinsic factors comprise individual characteristics, such as genetic predisposition and hormonal fluctuations․ Extrinsic factors encompass environmental influences, including stress, dietary habits, and exposure to certain medications․
These factors can disrupt the normal functioning of the pilosebaceous unit, leading to an overproduction of sebum, an oily substance that clogs pores and fosters the growth of Propionibacterium acnes (P․ acnes)․ The interaction between these elements creates an environment conducive to acne development․ Elucidating the causes of adult acne is essential for the implementation of effective therapeutic strategies and prevention of future breakouts․
A comprehensive understanding of the causal factors underlying adult acne is crucial for the development of targeted treatments and improved management of this debilitating condition․ By examining the interplay of intrinsic and extrinsic factors, researchers and clinicians can work towards providing optimal care for individuals affected by adult acne․
Hormonal Imbalance
Hormonal fluctuations play a pivotal role in the development of adult acne․ Androgens, such as testosterone, stimulate the sebaceous glands, leading to an increase in sebum production․ This surge in sebum can clog pores and create an environment conducive to acne formation․
In women, hormonal imbalances can occur due to various factors, including polycystic ovary syndrome (PCOS), menstruation, pregnancy, and menopause․ These hormonal shifts can disrupt the delicate balance of androgens and estrogens, leading to acne-prone skin․
Furthermore, hormonal imbalances can also affect insulin sensitivity, leading to increased inflammation and oxidative stress․ This, in turn, can exacerbate acne symptoms․ A thorough understanding of the interplay between hormones and acne is essential for the development of targeted therapeutic strategies․
Research has shown that hormonal therapies, such as spironolactone, can be effective in treating adult acne in women․ Additionally, lifestyle modifications, including dietary changes and stress management, can also help to mitigate the impact of hormonal imbalances on acne-prone skin․
By addressing hormonal imbalances, individuals can take a crucial step towards achieving clearer, healthier skin and reducing the occurrence of adult acne․
Stress
Stress is a ubiquitous aspect of modern life, and its impact on the skin should not be underestimated․ The relationship between stress and acne is complex, involving multiple physiological pathways․
When an individual experiences stress, their body responds by releasing stress hormones, such as cortisol and adrenaline․ These hormones stimulate the sebaceous glands, leading to increased sebum production and, subsequently, acne․
Furthermore, stress can also impair the skin’s natural barrier function, making it more susceptible to inflammation and infection․ This can lead to the formation of acne lesions, including papules, pustules, and nodules․
Research has shown that individuals with acne-prone skin exhibit heightened stress responses, suggesting a bidirectional relationship between stress and acne․ Effective stress management techniques, such as meditation, yoga, and deep breathing exercises, can help mitigate the negative impact of stress on the skin․
By acknowledging the role of stress in adult acne, individuals can take proactive steps to manage their stress levels and reduce the occurrence of acne breakouts, ultimately leading to healthier, more radiant skin․
A holistic approach to skincare, incorporating stress management and relaxation techniques, is essential for achieving optimal results in the treatment of adult acne․
Genetics
Genetic predisposition plays a significant role in adult acne development․ Individuals with a family history of acne are more likely to experience breakouts, as inherited traits can affect sebum production, skin texture, and inflammation response․
Skin Care Routine and Adult Acne
A well-established skin care routine is crucial in preventing and managing adult acne․ However, certain products and practices can exacerbate the condition․ Using comedogenic products, which clog pores, can lead to acne development․ Furthermore, over-exfoliating or using harsh products can strip the skin of its natural oils, causing irritation and inflammation․
Additionally, failing to remove makeup properly or using expired products can also contribute to adult acne․ A consistent and gentle skin care routine, tailored to individual skin types, is essential in maintaining healthy skin․ This includes using non-comedogenic products, cleansing the skin twice daily, and applying sunscreen regularly․ By adopting a suitable skin care routine, individuals can significantly reduce their risk of developing adult acne and alleviate existing symptoms․
It is also important to note that skin care routines should be adapted to individual skin concerns and needs․ Consulting a dermatologist can help determine the best course of treatment and recommend personalized skin care regimens․
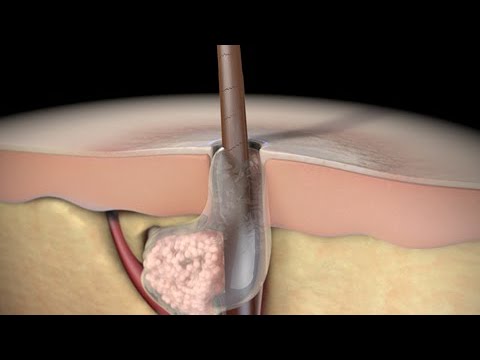
Clogged Pores
Clogged pores are a primary contributor to the development of adult acne․ When dead skin cells, oil, and other debris accumulate in the pores, they can cause blockages that lead to inflammation and acne․ There are several factors that can contribute to clogged pores, including excessive sebum production, poor skin care habits, and environmental factors such as pollution and humidity․
When pores become clogged, bacteria can multiply, leading to infection and inflammation․ This can cause a range of symptoms, from mild blackheads and whiteheads to severe cystic acne․ Furthermore, clogged pores can also lead to the formation of acne scars, which can be difficult to treat and may have a lasting impact on the skin’s appearance․
Understanding the role of clogged pores in adult acne is crucial for effective prevention and treatment․ By taking steps to prevent pore clogging, such as using non-comedogenic products and exfoliating regularly, individuals can reduce their risk of developing adult acne and maintain healthier, clearer skin․
Bacteria Growth
The proliferation of bacteria, particularly Propionibacterium acnes (P․ acnes), within clogged pores can exacerbate adult acne․ Bacteria feed on sebum, producing waste products that stimulate inflammation and worsen acne symptoms․
Inflammation and Breakouts
Inflammation plays a pivotal role in the development of adult acne․ When pores become clogged with dead skin cells, oil, and bacteria, the surrounding skin tissue becomes inflamed, leading to the characteristic redness and swelling associated with acne․
This inflammatory response is a natural defense mechanism, attempting to eliminate the perceived threat․ However, in the case of adult acne, it can have detrimental effects, causing further irritation and scarring․
As inflammation intensifies, the pore wall can rupture, releasing its contents into the surrounding tissue․ This leads to the formation of papules, pustules, and cysts, which are hallmarks of adult acne․
Understanding the complex interplay between inflammation and breakouts is essential for developing effective treatment strategies․ By addressing the underlying causes of inflammation, individuals can reduce the severity and frequency of adult acne episodes, ultimately achieving clearer, healthier-looking skin․
A comprehensive approach, incorporating lifestyle modifications, topical treatments, and professional interventions, can help mitigate the impact of inflammation and breakouts, restoring confidence and overall well-being․
The Role of Inflammation
Inflammation is a multifaceted process that contributes significantly to the pathogenesis of adult acne․ The inflammatory cascade involves the activation of various cellular and molecular pathways, which converge to produce a complex response․
Key players in this process include pro-inflammatory cytokines, chemokines, and enzymes, which orchestrate the recruitment of immune cells to the site of inflammation․ These immune cells, such as neutrophils and macrophages, release reactive oxygen species and other mediators that exacerbate tissue damage․
The inflammatory response also promotes the formation of comedones, the primary lesions of acne, by increasing the expression of adhesion molecules and enhancing the migration of keratinocytes․ Furthermore, inflammation can lead to the production of post-inflammatory hyperpigmentation, resulting in persistent skin discoloration․
Elucidating the mechanisms underlying inflammation in adult acne is essential for the development of novel therapeutic strategies aimed at modulating this response․ By targeting specific components of the inflammatory cascade, clinicians may be able to improve treatment outcomes and reduce the risk of long-term sequelae․
Ongoing research continues to uncover the intricacies of inflammation in adult acne, paving the way for more effective management of this ubiquitous skin condition․
Breakouts and Pimples
Breakouts and pimples are characteristic manifestations of adult acne, presenting as erythematous papules, pustules, or nodules․ These lesions can be painful, tender, and disfiguring, significantly impacting an individual’s quality of life and self-esteem․
Treating Adult Acne
The treatment of adult acne necessitates a comprehensive approach, incorporating both pharmacological and non-pharmacological interventions․ A thorough assessment of the patient’s medical history, skin type, and acne severity is crucial in determining the most effective treatment strategy․
A variety of topical and systemic agents are available, including retinoids, benzoyl peroxide, salicylic acid, and antibiotics․ These agents target various pathogenic factors, such as comedogenesis, bacterial proliferation, and inflammation․
In addition to pharmacological interventions, patients may benefit from non-pharmacological treatments, including blue light therapy, extractions, and lifestyle modifications․ A well-structured treatment plan, tailored to the individual’s specific needs and skin characteristics, is essential in achieving optimal outcomes․
Regular follow-up appointments with a dermatologist are vital in monitoring treatment efficacy, addressing potential side effects, and making necessary adjustments to the treatment regimen․ By adopting a patient-centered approach, clinicians can significantly improve the management of adult acne, reducing the physical and emotional burden associated with this condition․
Dermatology and Acne Treatments
Dermatologists play a pivotal role in the diagnosis and management of adult acne․ A comprehensive dermatological assessment enables the identification of underlying causes, such as hormonal imbalances, and the development of personalized treatment plans․
Topical retinoids, derived from vitamin A, are commonly prescribed for their ability to prevent comedone formation and reduce inflammation․ Benzoyl peroxide and salicylic acid are also frequently employed, due to their bactericidal and comedolytic properties․
For more severe cases, systemic treatments, such as oral antibiotics and isotretinoin, may be necessary․ These agents target the underlying causes of acne, including bacterial proliferation and inflammation․
In addition to pharmacological interventions, dermatologists may recommend adjunctive therapies, such as blue light treatment and extractions, to enhance treatment efficacy․ By leveraging their expertise in dermatology, clinicians can provide patients with effective, evidence-based treatments, ultimately improving the management of adult acne and mitigating its impact on quality of life․
A collaborative approach between the patient and dermatologist is essential in achieving optimal outcomes and minimizing potential side effects․
Preventing Future Breakouts
To prevent future breakouts, maintaining a consistent skincare routine, using non-comedogenic products, and avoiding picking or popping pimples is crucial․ Regular follow-up appointments with a dermatologist can also help identify and address emerging issues․
In conclusion, adult acne is a complex condition influenced by a multitude of factors, including hormonal imbalances, stress, genetics, and skincare routines․ Understanding the underlying causes of adult acne is essential for effective management and treatment․ By recognizing the interplay between these factors, individuals can take proactive steps to mitigate their impact and reduce the occurrence of breakouts․
A comprehensive approach to adult acne treatment involves a combination of medical therapies, lifestyle modifications, and patient education․ By working together with healthcare professionals, individuals can develop personalized treatment plans tailored to their unique needs and circumstances․
Ultimately, adult acne is a treatable condition, and with the right guidance and support, individuals can achieve significant improvements in their skin health and overall quality of life․ By prioritizing education, awareness, and proactive management, we can empower individuals to take control of their adult acne and unlock a clearer, healthier complexion․
Final Thoughts
As we conclude our exploration of adult acne causes, it is essential to acknowledge the profound impact this condition can have on an individual’s self-esteem and overall well-being․ The emotional toll of living with adult acne should not be underestimated, and it is crucial to approach treatment with empathy and understanding․
By fostering a culture of openness and awareness, we can work to dispel the stigma surrounding adult acne and encourage individuals to seek help without fear of judgment․ Education and advocacy are key components in this effort, and it is our collective responsibility to promote a supportive and inclusive environment for those affected by this condition․
As research continues to uncover the intricacies of adult acne, we are reminded of the importance of ongoing investigation and innovation in the field of dermatology․ By pushing the boundaries of knowledge and treatment options, we can offer new hope and improved outcomes for individuals struggling with adult acne, ultimately enhancing their quality of life and empowering them to face the future with confidence․
I appreciated how this article aimed to educate readers without resorting to overly technical jargon or complicated explanations.
I appreciate how this article emphasizes the importance of understanding the causal factors underlying adult acne for effective treatment strategies. However, I would have liked more information on potential treatments.
The writing style is clear and concise, making it easy for non-experts to grasp complex concepts. I especially appreciated the explanation of how hormonal fluctuations contribute to adult acne.
As a dermatologist, I found this article informative but somewhat lacking in depth. While it covers key points well, it doesn
While informative overall, I felt some sections were slightly repetitive or overlapping; tightening up these areas could improve readability.
I liked how this article discussed both intrinsic and extrinsic factors contributing to adult acne. However, I felt that some sections could benefit from additional examples or illustrations.
This article provides a comprehensive overview of adult acne, highlighting its multifactorial nature and the interplay between intrinsic and extrinsic factors. The section on hormonal imbalance is particularly insightful.
Overall, this was an engaging read with useful insights into adult acne causes. One minor suggestion would be adding more transitional phrases between paragraphs for smoother flow.