Autosomal Dominant Polycystic Kidney Disease (ADPKD)⁚ A Comprehensive Overview
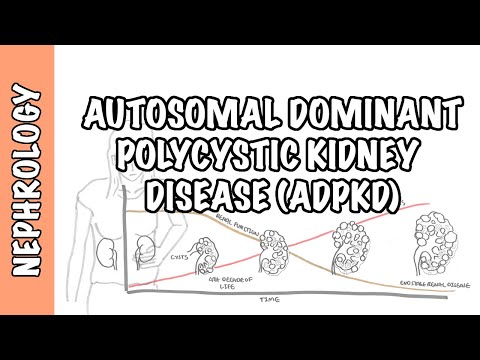
Autosomal dominant polycystic kidney disease (ADPKD) is a prevalent genetic disorder characterized by the development of multiple fluid-filled cysts within the kidneys‚ leading to chronic kidney damage.
Introduction
Autosomal dominant polycystic kidney disease (ADPKD) is a complex and multifaceted disorder that affects various aspects of an individual’s life. As one of the most common inherited disorders‚ ADPKD has significant implications for public health and the healthcare system. Characterized by the growth of numerous cysts filled with fluid in the kidneys‚ ADPKD can lead to chronic kidney damage‚ renal failure‚ and end-stage renal disease. The condition is often associated with significant morbidity‚ mortality‚ and reduced quality of life. Despite advances in medical research and technology‚ ADPKD remains a substantial clinical challenge. This comprehensive overview aims to provide an in-depth examination of the etiology‚ genetics‚ clinical presentation‚ diagnosis‚ complications‚ and management of ADPKD‚ as well as current research and future directions in the field. A thorough understanding of the disease is essential for the development of effective therapeutic strategies and improved patient outcomes.
Etiology and Genetics
The etiology of ADPKD is primarily attributed to genetic mutations in the PKD1 and PKD2 genes‚ which encode for polycystin-1 and polycystin-2‚ crucial proteins in maintaining renal tubular structure.
Genetic Basis of ADPKD
The genetic basis of autosomal dominant polycystic kidney disease (ADPKD) involves mutations in two distinct genes⁚ PKD1 and PKD2. These genes are responsible for encoding the proteins polycystin-1 and polycystin-2‚ which play crucial roles in maintaining the structural integrity of renal tubules.
Mutations in the PKD1 gene account for approximately 85-90% of ADPKD cases‚ while PKD2 mutations are responsible for the remaining 10-15%. The genetic alterations lead to the production of aberrant polycystin proteins‚ disrupting normal cellular signaling pathways and ultimately resulting in the formation of cysts within the kidneys.
The genetic heterogeneity of ADPKD contributes to the variable expression of the disease‚ including differences in age of onset‚ rate of progression‚ and severity of symptoms. Elucidating the genetic basis of ADPKD has facilitated the development of molecular diagnostic techniques and enabled the identification of at-risk individuals.
Autosomal Dominant Inheritance
Autosomal dominant polycystic kidney disease (ADPKD) is characterized by an autosomal dominant pattern of inheritance‚ meaning that a single copy of the mutated gene is sufficient to cause the disease.
Each child of an affected parent has a 50% chance of inheriting the mutated gene‚ regardless of their sex. This results in a vertical pattern of inheritance‚ where the disease is passed from parent to child through generations.
The autosomal dominant nature of ADPKD is reflected in its familial clustering‚ with multiple affected family members often spanning several generations. The disease exhibits complete penetrance‚ meaning that all individuals who inherit the mutated gene will eventually develop ADPKD‚ although the age of onset and severity of symptoms may vary.
This predictable pattern of inheritance enables genetic counseling and facilitates the identification of at-risk individuals‚ allowing for early monitoring and intervention.
Clinical Presentation and Diagnosis
Clinical presentation of ADPKD varies widely‚ with some patients remaining asymptomatic until late adulthood‚ while others experience early-onset hypertension‚ hematuria‚ and abdominal pain due to cyst growth.
Symptoms and Signs
The symptoms and signs of autosomal dominant polycystic kidney disease (ADPKD) can vary widely in severity and age of onset. Many patients remain asymptomatic until adulthood‚ when cysts have grown large enough to cause noticeable symptoms. Common presenting complaints include abdominal pain‚ flank pain‚ or discomfort due to cyst growth or rupture. Hematuria‚ either microscopic or gross‚ is another frequent finding. Hypertension is a common and early manifestation of ADPKD‚ often preceding renal impairment. Other possible symptoms include urinary tract infections‚ kidney stones‚ and symptoms related to extrarenal manifestations‚ such as liver cysts‚ intracranial aneurysms‚ or cardiac valvular abnormalities. Some patients may also experience fatigue‚ weight loss‚ or nausea due to advanced renal disease or cyst-related complications. A thorough physical examination may reveal palpable abdominal masses or tenderness in the flanks.
Diagnostic Imaging and Testing
Diagnostic imaging plays a crucial role in the evaluation and diagnosis of autosomal dominant polycystic kidney disease (ADPKD). Ultrasonography is the primary imaging modality‚ allowing for the detection of cysts and assessment of kidney size. Computed tomography (CT) scans and magnetic resonance imaging (MRI) may also be utilized to further evaluate cyst characteristics‚ identify potential complications‚ and assess extrarenal manifestations. MRI is particularly useful for detecting liver cysts and evaluating the brain for intracranial aneurysms. Additionally‚ genetic testing may be employed to identify mutations in the PKD1 or PKD2 genes‚ which can confirm the diagnosis. Laboratory tests‚ including serum creatinine‚ electrolyte panels‚ and urinalysis‚ are used to assess renal function and monitor disease progression. Imaging and laboratory studies are essential for establishing a diagnosis‚ guiding management decisions‚ and monitoring disease progression in patients with ADPKD.
Complications and Management
Patients with ADPKD are at risk for various complications‚ including renal failure‚ hypertension‚ and cyst-related morbidity‚ necessitating comprehensive management strategies to mitigate these risks and improve quality of life.
Renal Failure and End-Stage Renal Disease
Renal failure is a common complication of ADPKD‚ resulting from the progressive expansion of cysts and subsequent destruction of normal renal parenchyma. As the disease advances‚ patients may progress to end-stage renal disease (ESRD)‚ necessitating renal replacement therapy. The rate of progression to ESRD varies widely among individuals‚ influenced by factors such as age‚ sex‚ and genetic background. In general‚ patients with ADPKD who have a family history of early-onset ESRD are more likely to experience rapid decline in renal function. Regular monitoring of renal function and timely initiation of dialysis or transplantation can significantly improve outcomes for patients with ADPKD-related ESRD. Furthermore‚ optimal management of hypertension‚ proteinuria‚ and other comorbid conditions can help slow the progression of renal disease and delay the onset of ESRD.
Management and Treatment Options
The management of ADPKD is primarily focused on slowing disease progression‚ controlling symptoms‚ and mitigating complications. Hypertension is aggressively managed through lifestyle modifications and pharmacotherapy to reduce the risk of cardiovascular disease and slow renal function decline. Pain management is also crucial‚ with options including analgesics‚ narcotics‚ and surgical interventions. Additionally‚ patients with ADPKD are advised to maintain a healthy lifestyle‚ including a balanced diet‚ regular exercise‚ and smoking cessation. For patients with advanced disease‚ renal replacement therapy‚ including hemodialysis‚ peritoneal dialysis‚ and kidney transplantation‚ may be necessary. Novel therapeutic agents‚ such as tolvaptan‚ have been approved for the treatment of ADPKD and have shown promise in reducing cyst growth and slowing disease progression. A multidisciplinary approach‚ involving nephrologists‚ urologists‚ and other healthcare professionals‚ is essential for providing comprehensive care to patients with ADPKD.
Current Research and Future Directions
Ongoing research focuses on elucidating molecular mechanisms underlying ADPKD‚ identifying novel therapeutic targets‚ and developing innovative treatments‚ including gene therapies and small-molecule inhibitors‚ to slow disease progression.
Molecular and Cellular Mechanisms
The molecular and cellular mechanisms underlying ADPKD involve a complex interplay between genetic and environmental factors. Mutations in the PKD1 and PKD2 genes‚ encoding polycystin-1 and polycystin-2‚ respectively‚ disrupt normal cell signaling and lead to aberrant cell proliferation and differentiation. Altered expression of various signaling molecules‚ including cAMP‚ mTOR‚ and STAT3‚ contributes to the development and progression of cysts. Additionally‚ changes in the extracellular matrix and altered interactions between cyst-lining epithelial cells and the surrounding stroma play critical roles in cyst growth and expansion. Elucidating these molecular and cellular mechanisms is essential for the development of effective therapeutic strategies targeting the root causes of ADPKD.
Emerging Therapies and Clinical Trials
Several emerging therapies and ongoing clinical trials hold promise for the treatment of ADPKD. Tolvaptan‚ a vasopressin V2 receptor antagonist‚ has shown efficacy in slowing cyst growth and reducing kidney volume. Other investigational agents‚ such as octreotide and lanreotide‚ aim to inhibit cyst growth by targeting somatostatin receptors. Additionally‚ novel approaches‚ including gene therapy and RNA interference‚ are being explored to address the underlying genetic defects. Clinical trials evaluating the safety and efficacy of these innovative treatments are underway. Furthermore‚ research into repurposed therapies‚ such as metformin and pioglitazone‚ may provide new avenues for managing ADPKD-related complications. As the field continues to evolve‚ patients with ADPKD may soon have access to a range of effective treatment options to slow disease progression and improve quality of life.
In conclusion‚ autosomal dominant polycystic kidney disease (ADPKD) is a complex and multifaceted disorder that requires comprehensive management and care. While significant progress has been made in understanding the genetic basis and pathophysiology of the disease‚ further research is needed to develop effective treatments and improve patient outcomes. Early diagnosis‚ regular monitoring‚ and timely interventions are crucial for slowing disease progression and preventing complications. A multidisciplinary approach‚ involving nephrologists‚ urologists‚ and other healthcare professionals‚ is essential for providing optimal care to patients with ADPKD. By continuing to advance our knowledge and understanding of this disease‚ we can work towards improving the quality of life and prognosis for individuals affected by ADPKD. Ultimately‚ a collaborative effort between researchers‚ clinicians‚ and patients is necessary to achieve better outcomes and develop a cure for this devastating disease.
Overall, this article is well-written and comprehensive, making it a valuable resource for clinicians, researchers, and students interested in learning about ADPKD.
I appreciate the detailed explanation of the genetic basis of ADPKD, including the role of PKD1 and PKD2 genes in encoding polycystin-1 and polycystin-2 proteins. However, I would have liked to see more discussion on potential therapeutic targets for these proteins.
While this article provides a thorough overview of ADPKD, I felt that it could benefit from more visual aids such as diagrams or illustrations to help explain complex concepts like cyst formation and renal tubular structure.
This article provides a comprehensive overview of Autosomal Dominant Polycystic Kidney Disease (ADPKD), covering its etiology, genetics, clinical presentation, diagnosis, complications, and management. The inclusion of current research and future directions in the field makes it a valuable resource for healthcare professionals.
As a nephrologist, I found this article to be informative and up-to-date on the latest research on ADPKD. The section on complications was particularly useful, highlighting the importance of monitoring patients for cardiovascular disease, hypertension, and other related conditions.
I appreciated the emphasis on public health implications and healthcare system burden associated with ADPKD. This highlights the need for increased awareness, early detection, and effective management strategies to improve patient outcomes.