Back of the Headache⁚ Understanding the Causes and Symptoms
The back of the headache is a prevalent condition characterized by recurring pain in the posterior region of the head, often accompanied by neck pain and stress. A comprehensive understanding of its causes and symptoms is crucial for effective management and treatment.
Introduction to Back of the Headache
The back of the headache is a complex and multifaceted condition that affects millions of individuals worldwide. Characterized by persistent or recurring pain in the posterior region of the head, this type of headache can significantly impact daily life, social interactions, and overall well-being.
Despite its prevalence, the back of the headache remains poorly understood, and its causes and symptoms are often misattributed or overlooked. As a result, many individuals suffer from inadequate treatment and management, leading to prolonged periods of discomfort and distress.
A thorough understanding of the back of the headache is essential for developing effective treatment strategies and improving patient outcomes. This requires a comprehensive approach that takes into account the intricate relationships between physical, emotional, and environmental factors that contribute to this condition.
By exploring the underlying mechanisms and characteristics of the back of the headache, healthcare professionals can provide more accurate diagnoses, targeted treatments, and personalized care plans that address the unique needs of each individual.
This article aims to provide an in-depth examination of the back of the headache, its causes, symptoms, and treatment options, serving as a valuable resource for both healthcare professionals and individuals affected by this debilitating condition.
Common Causes of Back of the Headache
Back of the headache is often attributed to a combination of physical and medical factors, including tension headache, migraines, and cluster headaches, as well as underlying conditions that affect the cervical spine and surrounding muscles.
Physical Causes⁚ Muscle Strain and Poor Posture
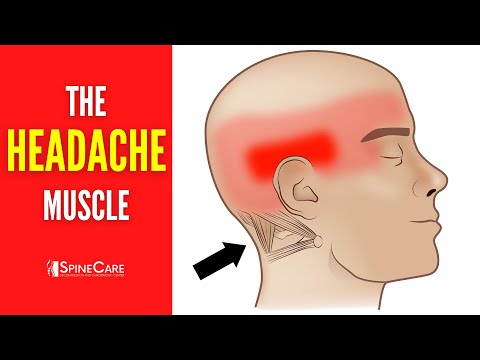
Physical causes of back of the headache can be attributed to muscle strain and poor posture. The muscles in the neck and scalp, particularly the suboccipital muscles, play a crucial role in maintaining proper alignment and movement of the head. When these muscles become strained or imbalanced, it can lead to pain and tension in the back of the head.
Poor posture is another significant contributor to back of the headache. When an individual maintains a forward head posture or rounded shoulders, it can put additional strain on the muscles in the neck and scalp, leading to discomfort and pain. Furthermore, prolonged sitting or standing in one position can also exacerbate muscle strain and poor posture, ultimately contributing to the development of back of the headache.
In order to address physical causes of back of the headache, it is essential to adopt proper posture and engage in regular stretching and strengthening exercises to maintain healthy muscle function. Additionally, taking regular breaks to move and stretch can help reduce muscle strain and alleviate symptoms associated with back of the headache.
Medical Conditions⁚ Tension Headache, Migraines, and Cluster Headaches
Certain medical conditions can contribute to the development of back of the headache. Tension headache, for instance, is a common condition characterized by a dull, aching pain in the head, often accompanied by neck pain and tension in the scalp.
Migraines are another medical condition that can cause back of the headache. These severe headaches are typically accompanied by sensitivity to light and sound, nausea, and vomiting. In some cases, migraines can cause pain on one side of the head, including the back of the head.
Cluster headaches are a rare but severe type of headache that can also cause back of the headache. These headaches occur in clusters or cycles, often waking individuals from sleep. The pain associated with cluster headaches is typically intense and piercing, often localized to one side of the head, including the back of the head. Understanding the underlying medical condition is crucial for effective management and treatment of back of the headache.
A thorough diagnosis by a healthcare professional is necessary to determine the underlying medical condition contributing to back of the headache and develop a personalized treatment plan to alleviate symptoms.
Other Contributing Factors
In addition to physical and medical causes, other factors can contribute to the development of back of the headache, including environmental and lifestyle factors that affect the cervical spine and surrounding muscles, leading to pain and discomfort.
Sinus Pressure and Cervical Spine Issues
Sinus pressure and cervical spine issues can significantly contribute to the development of back of the headache. The sinuses are air-filled cavities located in the skull, and when they become inflamed or infected, it can lead to sinus pressure and pain in the face, forehead, and back of the head.
Cervical spine issues, such as herniated discs, spinal stenosis, or degenerative disc disease, can also cause back of the headache. The cervical spine is composed of seven vertebrae, and any abnormality in this region can put pressure on the surrounding nerves and muscles, leading to pain and discomfort.
The suboccipital muscles, which connect the base of the skull to the top of the neck, play a crucial role in maintaining proper posture and movement of the head and neck. When these muscles become strained or inflamed, it can lead to pain and stiffness in the back of the head and neck. A thorough evaluation by a healthcare professional is necessary to determine the underlying cause of back of the headache and develop an effective treatment plan.
Occipital Neuralgia⁚ A Common Cause of Back of the Headache
Occipital neuralgia is a type of headache disorder characterized by intense, stabbing pain in the back of the head, often accompanied by tenderness and sensitivity to light touch. This condition occurs when the occipital nerves, which run from the base of the skull to the scalp, become inflamed or irritated.
The pain associated with occipital neuralgia is typically unilateral, meaning it affects one side of the head, and can be exacerbated by movement, tension, or pressure on the affected area. In some cases, patients may experience pain or numbness in the face, neck, or shoulders, as well as sensitivity to light and sound.
A diagnosis of occipital neuralgia is typically made through a combination of physical examination, medical history, and diagnostic tests, such as nerve blocks or imaging studies. Treatment options for occipital neuralgia may include medications, physical therapy, and interventional procedures, such as nerve blocks or radiofrequency ablation. In some cases, lifestyle modifications, such as stress management and ergonomic changes, may also be recommended to help manage symptoms and prevent exacerbations.
Treatment Options for Back of the Headache
A variety of treatment options are available to manage back of the headache, including pharmacological interventions, physical therapy, and alternative therapies. A comprehensive treatment plan should be tailored to the individual’s specific needs and underlying causes of their symptoms.
Trigger Point Therapy⁚ A Effective Treatment Option
Trigger point therapy is a highly effective treatment option for back of the headache, particularly when muscle strain and poor posture are contributing factors. This technique involves applying gentle, sustained pressure to specific areas of the muscle to release tension and alleviate pain.
The suboccipital muscles, located at the base of the skull, are a common area of tension that can contribute to back of the headache. Trigger point therapy can be used to target these muscles, releasing tension and promoting relaxation.
A licensed therapist will use a combination of manual techniques, including massage and joint mobilization, to identify and release trigger points in the affected muscles. Regular sessions can help to reduce the frequency and severity of back of the headache, improving overall quality of life.
It is essential to work with a qualified healthcare professional to develop a personalized treatment plan that incorporates trigger point therapy. With proper treatment, individuals can experience significant relief from back of the headache and improve their overall well-being.
Excellent job at explaining such complicated material simple terms though perhaps inclusion visual aids diagrams pictures might help solidify concepts readers unfamiliar anatomy physiology involved headaches generally.
While I agree with most points made here one area could benefit further exploration – discussion around preventive measures beyond conventional treatments considering lifestyle modifications dietary changes etc could add significant value
What I appreciate most about this article isn’t just information presented but clear compassionate tone used addressing sufferers directly rather than merely treating them statistics
This article provides an excellent introduction to understanding back headaches; however I would have liked to see more specific examples or case studies illustrating how these concepts apply in real-world scenarios.
As someone who has suffered from chronic headaches myself I found this piece incredibly informative; it effectively breaks down complex medical jargon making it accessible even for those without extensive medical backgrounds