Introduction to Hypertension and Its Treatment
Hypertension, a major risk factor for cardiovascular disease, necessitates effective management through antihypertensive drug therapy. Various classes of medications, including diuretics, beta blockers, and ACE inhibitors, are employed to regulate blood pressure and mitigate associated risks.
Understanding the Role of Diuretics
Diuretics are a fundamental class of antihypertensive medications that play a crucial role in managing high blood pressure. By increasing urine production, diuretics help eliminate excess fluid from the body, thereby reducing blood volume and alleviating pressure on the blood vessels.
The primary mechanism of action of diuretics involves inhibiting the reabsorption of sodium and chloride ions in the kidneys, leading to increased sodium and water excretion. This results in a decrease in blood volume, which in turn lowers blood pressure.
Diuretics are often used as first-line treatment for hypertension due to their efficacy and relatively low cost. They are particularly effective in patients with volume-dependent hypertension, such as those with edema or congestive heart failure. Additionally, diuretics can be used in combination with other antihypertensive medications to enhance their effects and achieve optimal blood pressure control.
Overall, diuretics are an essential component of antihypertensive therapy, offering a simple yet effective approach to managing high blood pressure and mitigating the associated risks of cardiovascular disease.
How Diuretics Help Lower Blood Pressure
Diuretics decrease blood pressure by reducing blood volume and cardiac preload, which in turn lowers systemic vascular resistance, resulting in decreased peripheral artery pressure and alleviated strain on the cardiovascular system, promoting overall cardiovascular health.
Beta Blockers⁚ A Critical Antihypertensive Drug Class
Beta blockers are a vital component of antihypertensive treatment regimens, offering a multifaceted approach to blood pressure management. By inhibiting the effects of catecholamines, such as epinephrine and norepinephrine, beta blockers reduce cardiac contractility, heart rate, and vascular resistance.
This pharmacological action results in decreased cardiac output, lower peripheral artery pressure, and reduced strain on the cardiovascular system. The benefits of beta blockers extend beyond blood pressure reduction, as they also mitigate the risk of cardiovascular complications, including myocardial infarction, stroke, and congestive heart failure.
The efficacy and safety of beta blockers have been extensively documented in clinical trials, solidifying their position as a cornerstone of hypertension management. Moreover, the availability of various beta blocker agents, each with distinct properties and indications, allows for tailored treatment strategies to meet the unique needs of individual patients. As a result, beta blockers remain a crucial element in the therapeutic arsenal against hypertension.
The Mechanism of Beta Blockers in Hypertension Management
Beta blockers competitively bind to beta-adrenergic receptors, inhibiting catecholamine-induced increases in heart rate, contractility, and vascular tone. This results in decreased cardiac output, reduced peripheral resistance, and subsequently, lower blood pressure levels.
ACE Inhibitors and Their Role in Cardiovascular Health
Angiotensin-converting enzyme (ACE) inhibitors are a pivotal class of medications in the management of hypertension and cardiovascular disease. By inhibiting the conversion of angiotensin I to angiotensin II, ACE inhibitors effectively reduce peripheral resistance and lower blood pressure.
The renin-angiotensin-aldosterone system (RAAS) plays a crucial role in regulating blood pressure, fluid balance, and electrolyte homeostasis. ACE inhibitors disrupt this cascade, resulting in decreased levels of angiotensin II, a potent vasoconstrictor. This reduction in angiotensin II leads to vasodilation, natriuresis, and diuresis, ultimately contributing to decreased blood pressure.
Furthermore, ACE inhibitors have been shown to possess additional cardiovascular protective effects, including improved ventricular function, enhanced nitric oxide production, and inhibition of apoptosis. These benefits contribute to their utility in treating heart failure, post-myocardial infarction, and other cardiovascular conditions. As such, ACE inhibitors remain an essential component of antihypertensive therapy, promoting optimal cardiovascular health and reducing the risk of associated morbidities.
How ACE Inhibitors Promote Vasodilation and Reduce Blood Pressure
ACE inhibitors facilitate vasodilation by reducing angiotensin II levels, thereby decreasing peripheral resistance and promoting relaxed vascular tone, which in turn lowers blood pressure and improves cardiovascular hemodynamics, mitigating the risks associated with hypertension.
Calcium Channel Blockers⁚ Facilitating Heart Disease Prevention
Calcium channel blockers (CCBs) are a crucial class of antihypertensive medications that have been extensively utilized in the management of hypertension. By selectively inhibiting the influx of calcium ions into vascular smooth muscle cells and cardiac muscle cells, CCBs induce vasodilation and reduce blood pressure.
The primary mechanism of action of CCBs involves the binding to L-type calcium channels, thereby preventing the depolarization of vascular smooth muscle cells and subsequent vasoconstriction. This results in decreased peripheral resistance, reduced cardiac workload, and improved cardiovascular hemodynamics.
In addition to their antihypertensive effects, CCBs have been shown to exhibit anti-atherogenic properties, reducing the risk of cardiovascular events and facilitating heart disease prevention. The efficacy and safety of CCBs have been consistently demonstrated in numerous clinical trials, solidifying their position as a valuable therapeutic option in the management of hypertension and associated cardiovascular risk factors.
As a result, CCBs are widely recommended as a first-line treatment for patients with hypertension, particularly those with concomitant conditions such as angina pectoris or Raynaud’s disease.
Calcium Channel Blockers⁚ Mechanism of Action
Calcium channel blockers bind to L-type calcium channels, preventing calcium ion influx into vascular smooth muscle cells and cardiac muscle cells, thereby inducing vasodilation, reducing peripheral resistance, and ultimately lowering blood pressure effectively.
Vasodilators⁚ Directly Lowering Blood Pressure
Vasodilators are a class of antihypertensive medications that directly relax the smooth muscle cells of blood vessels, causing vasodilation and a subsequent reduction in peripheral resistance. This decrease in resistance leads to a lowering of blood pressure.
The mechanism of action of vasodilators is multifaceted, involving the modulation of various signaling pathways and ion channels within vascular smooth muscle cells. By increasing the diameter of blood vessels, vasodilators facilitate increased blood flow and reduced blood pressure.
Vasodilators can be further categorized into two primary subtypes⁚ arterial dilators and venous dilators. Arterial dilators primarily affect the arterioles, reducing systemic vascular resistance, whereas venous dilators target the venules, decreasing venous return and cardiac preload. The judicious use of vasodilators as part of a comprehensive treatment plan can effectively manage hypertension and mitigate associated cardiovascular risks.
In clinical practice, vasodilators are often employed in combination with other antihypertensive agents to achieve optimal blood pressure control. Their direct vasodilatory effects make them a valuable adjunct in the management of hypertension, particularly in patients with refractory or resistant hypertension.
Vasodilators⁚ A Direct Approach to Managing Hypertension
Vasodilators offer a targeted approach to hypertension management by directly relaxing vascular smooth muscle, reducing peripheral resistance, and promoting blood vessel dilation, thereby rapidly lowering blood pressure and alleviating associated cardiovascular risks.
Combination Therapy⁚ Maximizing Antihypertensive Effects
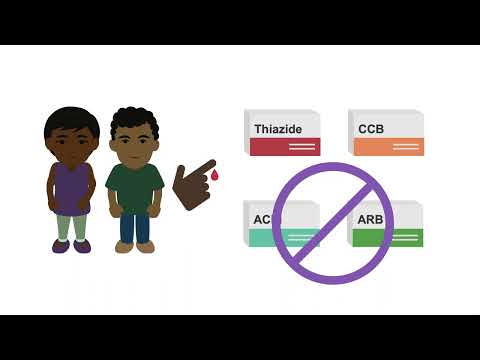
Combination therapy represents a cornerstone in the management of hypertension, particularly in patients with complex or resistant disease. By concurrently administering multiple antihypertensive agents with distinct mechanisms of action, clinicians can achieve enhanced blood pressure control and improved cardiovascular outcomes.
The rationale underlying combination therapy lies in its ability to target various physiological pathways implicated in blood pressure regulation, thereby mitigating counterregulatory responses and fostering additive or synergistic effects. This approach enables the use of lower doses of individual medications, reducing the risk of adverse events and enhancing patient adherence.
Clinical trials have consistently demonstrated the efficacy of combination therapy in achieving tighter blood pressure control and reducing the risk of major cardiovascular events. As such, combination therapy has become an integral component of modern antihypertensive treatment strategies, offering a tailored approach to managing hypertension and promoting optimal cardiovascular health.
The Importance of Customized Treatment Plans
Customized treatment plans are crucial in hypertension management, as individual patients exhibit unique profiles of risk factors, comorbidities, and responses to therapy, necessitating tailored approaches to optimize blood pressure control and minimize adverse events.
Managing Hypertension with Medication
The management of hypertension through medication is a multifaceted approach that requires careful consideration of individual patient needs and circumstances. By understanding the various classes of antihypertensive medications, including their mechanisms of action, indications, and potential side effects, healthcare providers can develop effective treatment plans that optimize blood pressure control and minimize adverse events.
Ultimately, the goal of antihypertensive therapy is to reduce the risk of cardiovascular morbidity and mortality, while also improving quality of life for individuals with hypertension. By working collaboratively with patients and engaging in ongoing monitoring and evaluation, healthcare providers can help achieve this goal and promote optimal cardiovascular health.
As new research and technologies continue to emerge, it is essential that healthcare providers stay up-to-date on the latest developments in antihypertensive therapy, ensuring that patients receive the most effective and evidence-based care possible. By doing so, we can continue to advance the management of hypertension and improve outcomes for individuals affected by this prevalent and debilitating condition.
Final Thoughts on Antihypertensive Drug Therapy
In conclusion, antihypertensive drug therapy plays a vital role in the management of hypertension, enabling individuals to control their blood pressure and mitigate the associated risks. As the prevalence of hypertension continues to rise, it is essential that healthcare providers are equipped with a comprehensive understanding of the various antihypertensive medications available.
Effective treatment plans must be tailored to individual patient needs, taking into account factors such as comorbidities, lifestyle, and medication tolerance. Furthermore, ongoing monitoring and evaluation are crucial to ensuring optimal blood pressure control and minimizing adverse events.
As research continues to advance our understanding of hypertension and its treatment, it is essential that healthcare providers remain informed and up-to-date on the latest developments. By working collaboratively with patients and engaging in evidence-based practice, we can promote optimal cardiovascular health and improve outcomes for individuals affected by hypertension. Through a commitment to excellence in antihypertensive therapy, we can make a meaningful difference in the lives of those we serve.
This article provides a comprehensive overview of hypertension and its treatment options. The explanation of diuretics
The article
I appreciate how the article highlights the importance of diuretics as a first-line treatment for hypertension. The discussion on their efficacy and low cost is well-supported.
As a healthcare professional, I appreciate the article
I found the section on diuretics
While the article provides a good introduction to beta blockers, I would have liked to see more information on their specific mechanisms of action and potential side effects.
While the article provides a solid foundation for understanding hypertension treatment, I think it would benefit from more discussion on emerging trends and research in antihypertensive therapy.
The section on how diuretics help lower blood pressure is clear and concise. The use of technical terms like “cardiac preload” and “systemic vascular resistance” adds credibility to the article.