Benign Paroxysmal Positional Vertigo⁚ An Overview
Benign paroxysmal positional vertigo (BPPV) is a vestibular disorder arising in the inner ear, characterized by brief yet intense episodes of vertigo triggered by specific head movements, often necessitating prompt medical evaluation and targeted intervention․
Definition and Prevalence
Benign paroxysmal positional vertigo (BPPV) is defined as a mechanical disorder of the inner ear, specifically affecting the vestibular system, where the movement of calcium particles (otoconia) within the semicircular canals induces vertiginous symptoms․ This condition is characterized by brief, episodic, and intense vertigo attacks, typically lasting seconds to minutes, and is often accompanied by nausea and vomiting․
The prevalence of BPPV is notable, with studies suggesting that it affects approximately 2․4% of the general population, increasing with age, and peaking in individuals between 50 to 70 years old․ Women are more likely to experience BPPV than men, and the condition often presents unilaterally, although bilateral involvement can occur․ BPPV may be idiopathic or secondary, resulting from head trauma, inner ear infections, or other ear disorders․ Its impact on quality of life is substantial, necessitating prompt diagnosis and effective management to alleviate symptoms and reduce the risk of falls and related injuries․
Understanding the definition and prevalence of BPPV is crucial for clinicians to recognize its clinical presentation, make accurate diagnoses, and provide timely interventions to improve patient outcomes and reduce the burden of this debilitating condition․
Clinical Presentation
Patients with benign paroxysmal positional vertigo typically exhibit a distinctive clinical profile, characterized by a sudden onset of intense, episodic vertigo, often accompanied by nausea, vomiting, and nystagmus, precipitated by specific head movements or positional changes․
Vertigo Symptoms and Balance Problems
Patients with benign paroxysmal positional vertigo (BPPV) often present with a range of vertigo symptoms and balance problems, which can significantly impact their quality of life․ The primary complaint is typically brief, intense episodes of vertigo, lasting from seconds to minutes․
These episodes are usually precipitated by specific head movements or positional changes, such as rolling over in bed, getting up from a lying down position, or looking up or down․ The vertigo symptoms can be accompanied by nausea, vomiting, and nystagmus, which can be debilitating for some patients․
In addition to vertigo, patients with BPPV may also experience balance problems, including unsteadiness, instability, and a tendency to veer to one side while walking․ These balance issues can increase the risk of falls, particularly in older adults, making it essential to address the underlying cause of the symptoms․
A thorough evaluation of the patient’s symptoms and medical history is crucial in determining the diagnosis and developing an effective treatment plan․ By understanding the specific characteristics of the vertigo symptoms and balance problems, healthcare professionals can tailor their approach to meet the unique needs of each patient․
Dizzy Spells and Inner Ear Disorder
Benign paroxysmal positional vertigo (BPPV) is characterized by recurrent dizzy spells that are directly related to an inner ear disorder․ The inner ear contains the vestibular system, which is responsible for maintaining balance and spatial orientation․
In BPPV, small calcium particles called otoconia become dislodged from their normal location in the vestibule and migrate into one of the semicircular canals․ This abnormal movement of the otoconia disrupts the normal functioning of the vestibular system, leading to the characteristic dizzy spells․
The dizzy spells in BPPV are often described as intense, brief episodes of vertigo that are triggered by specific head movements․ These episodes can be debilitating and disrupt a person’s daily activities․ The inner ear disorder underlying BPPV can also cause nausea, vomiting, and nystagmus, further exacerbating the symptoms․
Understanding the relationship between the dizzy spells and the inner ear disorder is crucial in developing an effective treatment plan for BPPV․ By addressing the underlying cause of the symptoms, healthcare professionals can help alleviate the dizzy spells and improve the patient’s overall quality of life․
A thorough evaluation of the patient’s symptoms and medical history is necessary to confirm the diagnosis of BPPV and rule out other potential causes of the dizzy spells․
Diagnosis and Treatment
Accurate diagnosis and effective treatment of benign paroxysmal positional vertigo (BPPV) require a comprehensive clinical evaluation, utilization of diagnostic tests, and implementation of targeted therapeutic interventions, often involving otolaryngology specialists and vestibular rehabilitation experts․
Positional Vertigo Diagnosis and Otolaryngology Treatment
Diagnosing positional vertigo involves a thorough medical history, physical examination, and diagnostic tests, including the Dix-Hallpike maneuver and electronystagmography (ENG)․ Otolaryngologists play a crucial role in evaluating and managing benign paroxysmal positional vertigo (BPPV) patients․
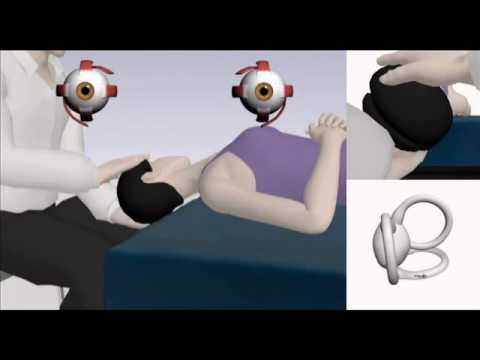
The primary objective of otolaryngology treatment for BPPV is to alleviate symptoms, restore vestibular function, and improve quality of life․ Treatment options may include the Epley maneuver, Semont maneuver, and Brandt-Daroff exercises, which aim to reposition and stabilize otoliths in the inner ear․
Otolaryngologists may also prescribe medications, such as antihistamines, anticholinergics, or benzodiazepines, to manage vertigo symptoms, although their use is generally limited due to potential side effects․ In some cases, intratympanic injections of gentamicin or corticosteroids may be administered to reduce vestibular function and alleviate symptoms․
A multidisciplinary approach, involving collaboration between otolaryngologists, audiologists, and physical therapists, is often necessary to ensure optimal treatment outcomes for patients with BPPV․ Regular follow-up appointments and monitoring of symptoms are essential to adjust treatment plans and prevent recurrence․
Early diagnosis and effective treatment can significantly improve the quality of life for patients with positional vertigo, enabling them to resume daily activities and maintain their independence․
Labyrinthitis and Vestibular Rehabilitation Therapy
Labyrinthitis, an inner ear disorder characterized by inflammation of the labyrinth, can be a contributing factor to benign paroxysmal positional vertigo (BPPV)․ In such cases, vestibular rehabilitation therapy (VRT) plays a vital role in promoting recovery and alleviating symptoms․
VRT is a customized exercise program designed to improve vestibular function, balance, and overall physical fitness․ A qualified physical therapist or audiologist works closely with the patient to develop a personalized treatment plan, incorporating exercises that challenge the vestibular system and promote adaptation․
The primary goals of VRT for labyrinthitis-related BPPV include enhancing vestibular compensation, reducing dizziness and vertigo, and improving balance and functional abilities․ Through a combination of habituation exercises, gaze stabilization techniques, and balance training, patients can experience significant improvements in their symptoms and quality of life․
Regular VRT sessions, often conducted over several weeks or months, are necessary to achieve optimal results․ Patients are also encouraged to practice exercises at home and incorporate lifestyle modifications to support their recovery and reduce the risk of recurrence․
By integrating VRT into the treatment plan, individuals with labyrinthitis-related BPPV can regain control over their symptoms and improve their overall well-being, enabling them to resume daily activities with confidence and independence․
Management and Outcome
Effective management of benign paroxysmal positional vertigo (BPPV) is crucial to prevent recurrence, reduce symptoms, and improve quality of life, necessitating a multidisciplinary approach that incorporates medical treatment, vestibular rehabilitation, and lifestyle modifications to achieve optimal outcomes․
Canalith Repositioning Procedure and Treatment Outcomes
The canalith repositioning procedure (CRP) is a highly effective treatment for benign paroxysmal positional vertigo (BPPV), involving a series of gentle maneuvers to relocate otoconia in the affected semicircular canal․ By repositioning these calcium particles, CRP aims to alleviate vertigo symptoms and restore vestibular function․
Studies have consistently demonstrated the efficacy of CRP in resolving BPPV symptoms, with success rates ranging from 70% to 90%․ The procedure is typically performed in an outpatient setting, with most patients experiencing significant improvement within one to two sessions․
Treatment outcomes following CRP are generally favorable, with many patients reporting complete resolution of vertigo symptoms․ However, some individuals may require additional treatments or experience residual symptoms, emphasizing the importance of close follow-up and ongoing management․ Factors influencing treatment outcomes include the severity of symptoms, presence of underlying conditions, and patient adherence to post-procedure instructions․
As a non-invasive and relatively low-risk intervention, CRP has become a cornerstone in the management of BPPV, offering patients a safe and effective means of alleviating debilitating vertigo symptoms and improving overall quality of life․
Long-Term Prognosis and Recurrence Rate
Following successful treatment, the long-term prognosis for individuals with benign paroxysmal positional vertigo (BPPV) is generally favorable, with many patients experiencing complete resolution of symptoms․ However, a significant proportion of patients may experience recurrence, with reported rates ranging from 20% to 50% over a 5-year period․
Factors influencing the likelihood of recurrence include the presence of underlying conditions, such as osteoporosis or inner ear disorders, as well as patient age and overall health status․ In some cases, BPPV may be a recurring condition, requiring ongoing management and periodic treatment․
Despite the potential for recurrence, the vast majority of patients with BPPV are able to manage their symptoms effectively and maintain a high quality of life․ Regular follow-up appointments and prompt intervention in the event of symptom recurrence are essential in minimizing the impact of BPPV on daily activities and overall well-being․
In rare cases, persistent or recurrent BPPV may be associated with underlying conditions requiring further evaluation and treatment․ As such, ongoing monitoring and collaboration between healthcare providers are crucial in ensuring optimal outcomes for individuals with this condition․
The author
This article provides an excellent overview of Benign Paroxysmal Positional Vertigo (BPPV), covering its definition, prevalence, clinical presentation, and impact on quality of life. The author
I would have liked to see more information on treatment options for BPPV. While the article mentions targeted intervention
I appreciate how this article highlights the importance of prompt diagnosis and effective management of BPPV to alleviate symptoms and reduce the risk of falls and related injuries.
The section on clinical presentation is particularly well-written. It provides a comprehensive understanding of the symptoms experienced by patients with BPPV.