Introduction to Brain Death
Brain death, a profound and irreversible loss of cerebral function, poses significant clinical and ethical challenges. Characterized by the cessation of all brain activity, it differs fundamentally from coma and vegetative states, warranting precise understanding and definition.
Defining Brain Death
Brain death is characterized by the irreversible loss of all functions of the brain, including the brainstem. This condition is distinct from other states of altered consciousness, such as coma or vegetative state. The diagnosis of brain death is based on a comprehensive evaluation of clinical signs and, in some cases, additional testing.
The essential criteria for diagnosing brain death include⁚ (1) a clear cause of irreversible brain damage, (2) absence of responsiveness to stimuli, (3) absence of spontaneous movements or reflexes, and (4) absence of brainstem functions, such as pupillary, corneal, and oculovestibular reflexes.
A thorough understanding of these diagnostic criteria is essential for accurately identifying brain death and distinguishing it from other neurological conditions. Furthermore, a clear definition of brain death is crucial for informed decision-making regarding end-of-life care, organ donation, and the management of patients with severe neurological damage.
The definition of brain death has significant implications for clinical practice, medical ethics, and the law. Therefore, it is essential to approach this topic with clarity, precision, and a deep understanding of the underlying medical and scientific principles.
Cerebral Cortex and Neurological Damage
The cerebral cortex, the outermost layer of the brain, plays a critical role in processing sensory information, controlling movement, and facilitating thought, perception, and emotion. Damage to the cerebral cortex can result in significant cognitive and motor impairments, depending on the location and extent of the injury.
In the context of brain death, damage to the cerebral cortex is often extensive and irreversible, leading to a complete loss of cortical function. This can be caused by various factors, including traumatic brain injury, stroke, or cerebral hypoxia. The resulting neurological damage can be assessed through clinical examination, imaging studies, and electrophysiological tests.
A thorough understanding of the cerebral cortex and its role in neurological function is essential for evaluating the extent of brain damage and determining the diagnosis of brain death. The assessment of cortical function, along with brainstem function, is a critical component of the diagnostic process, allowing clinicians to accurately identify patients who have suffered irreversible brain damage and meet the criteria for brain death.
By examining the cerebral cortex and its relationship to neurological damage, clinicians can develop a more nuanced understanding of brain death and its underlying pathophysiology.
Criteria for Brain Death
Brain death is diagnosed based on the presence of coma, absence of brainstem reflexes, and lack of spontaneous respiration, confirmed through clinical examination, apnea testing, and electroencephalography or imaging studies, as outlined in established medical guidelines.
Distinctions from Other Conditions
Distinguishing brain death from other altered states of consciousness is crucial for accurate diagnosis and treatment. The complexity of these conditions necessitates a comprehensive understanding of their distinct characteristics.
A range of disorders, including coma, vegetative state, and locked-in syndrome, can be mistaken for brain death due to similarities in clinical presentation. However, each of these conditions has unique features that set it apart from brain death.
A nuanced approach to diagnosis, incorporating clinical evaluation, laboratory tests, and imaging studies, is essential for distinguishing between these conditions. By recognizing the distinct hallmarks of each disorder, clinicians can provide more accurate prognoses and tailor treatment strategies to meet the individual needs of patients.
Ultimately, a thorough understanding of the differences between brain death and other conditions is vital for delivering high-quality patient care, addressing the needs of families and caregivers, and navigating the complex medical and ethical issues that arise in these situations.
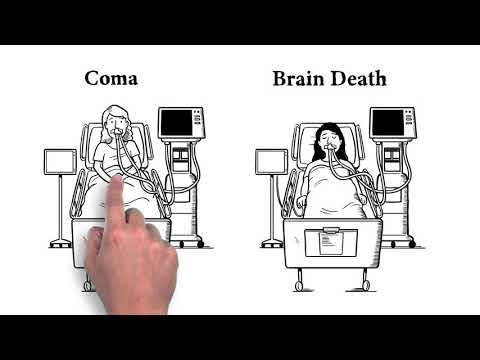
Coma vs. Brain Death
A coma is a state of profound unconsciousness, characterized by the absence of responsiveness to external stimuli. While coma patients may exhibit some brain activity, individuals who have suffered brain death display no cerebral function whatsoever.
The primary distinction between coma and brain death lies in the reversibility of the condition. Coma patients may regain consciousness, whereas brain death is an irreversible state. Furthermore, comatose patients often require ventilation and other life-sustaining interventions, but their brains continue to exhibit some level of activity.
In contrast, brain death is marked by the complete cessation of all brain function, including the brainstem. This results in the loss of all cranial nerve reflexes, respiratory drive, and other vital functions. The diagnosis of brain death is typically confirmed through a combination of clinical evaluation, laboratory tests, and imaging studies.
Understanding the differences between coma and brain death is essential for providing accurate prognoses, guiding treatment decisions, and addressing the emotional and psychological needs of patients’ families and caregivers.
Vegetative State and Locked-in Syndrome
Vegetative state and locked-in syndrome are distinct conditions characterized by preserved brainstem function, despite severe neurological damage. Patients in these states may exhibit spontaneous movements, eye opening, or even consciousness, but with profound cognitive impairment.
Implications of Brain Death
The diagnosis of brain death has profound implications for patients, families, and healthcare providers. It marks the end of all brain function, rendering the individual incapable of regaining consciousness or experiencing sensations. This irreversible loss of cerebral activity necessitates a reevaluation of treatment goals and the consideration of alternative care pathways.
As medical technology continues to advance, the possibilities for sustaining bodily functions in the absence of brain activity have increased, raising complex questions about the nature of life and death. The declaration of brain death serves as a critical juncture, beyond which the pursuit of curative interventions is no longer warranted.
In this context, the implications of brain death encompass not only the medical and technical aspects of care but also the emotional, social, and philosophical dimensions. A comprehensive understanding of these implications is essential for providing compassionate and informed support to those affected by this diagnosis.
Organ Donation and Medical Ethics
The diagnosis of brain death raises important questions regarding organ donation and the ethical considerations surrounding it. The irreversible loss of cerebral function provides a unique opportunity for individuals to contribute to the greater good through the donation of their organs.
Medical ethics dictate that organ procurement should only occur after the confirmation of brain death, as this ensures that the donor’s autonomy is respected and that the retrieval of organs does not cause harm to a potentially viable individual.
The process of organ donation following brain death must be conducted with transparency, dignity, and respect for the deceased and their loved ones. This includes obtaining informed consent from the donor or their surrogate decision-makers, ensuring that all relevant medical information is disclosed, and providing support to those who are grieving. By upholding these principles, the medical community can promote trust and confidence in the organ donation process, ultimately saving and improving lives through transplantation.
End-of-Life Care and Artificial Life Support
Following brain death, artificial life support may be continued to maintain organ perfusion for potential donation. However, this must be balanced with the need to provide dignified end-of-life care, respecting the individual’s autonomy and the family’s wishes.
In conclusion, brain death is a profound and irreversible condition that requires precise understanding and definition. It is essential to distinguish brain death from other states of altered consciousness, such as coma and vegetative state, in order to provide accurate diagnosis and appropriate care.
The implications of brain death are far-reaching, with significant consequences for organ donation, medical ethics, and end-of-life care. As such, it is crucial that healthcare professionals, patients, and families have a clear understanding of brain death and its connotations.
Ultimately, a comprehensive and compassionate approach to brain death is necessary, one that prioritizes the dignity and autonomy of the individual while also respecting the wishes and values of the family. By fostering a deeper understanding of brain death, we can work towards providing more effective and empathetic care for those affected by this complex and multifaceted condition.
Through ongoing education, research, and dialogue, we can continue to refine our understanding of brain death and its implications, ultimately enhancing the quality of care and support provided to individuals and families navigating this challenging and emotionally charged terrain.
Understanding Brain Death
To truly grasp the concept of brain death, it is essential to consider the intricacies of human consciousness and the complex interplay between the brain and the body. Brain death represents a distinct and irreversible loss of cerebral function, one that cannot be reversed by medical intervention or technological support.
A nuanced understanding of brain death requires an appreciation for the subtle yet critical distinctions between various states of altered consciousness. By recognizing the unique characteristics and clinical implications of brain death, healthcare professionals can provide more accurate diagnoses, effective care, and compassionate support to individuals and families navigating this challenging terrain.
Furthermore, a deeper understanding of brain death can inform and enrich discussions surrounding end-of-life care, organ donation, and medical ethics. By fostering a culture of awareness, empathy, and respect, we can work towards creating a more supportive and inclusive environment for those affected by brain death, ultimately promoting greater dignity, autonomy, and quality of life.
Through continued education, research, and open dialogue, we can cultivate a more profound understanding of brain death, one that honors the complexities of human existence and the inherent value of every individual life.
While I agree that clarity in defining brain death is crucial for medical ethics & law I wish there were specific examples illustrating real-world applications & disputes
One potential area for improvement could involve comparing international perspectives & varying legal definitions surrounding Brain Death.
What struck me most was how effectively this piece communicates intricate details without overwhelming readers – A testament to clear writing & solid structure
The section on cerebral cortex damage was particularly informative; however I would have liked more detailed explanations on potential causes.
I appreciate how this article emphasizes the importance of precise understanding and definition of brain death for informed decision-making regarding end-of-life care.
This article provides a comprehensive introduction to brain death, clearly defining its characteristics and distinguishing it from other states of altered consciousness.
This article demonstrates an impressive command over complex neuroscientific concepts while still being accessible to non-experts.
Excellent overview! Though perhaps further discussion on advancements & future directions within research could enhance reader engagement