Introduction to Diabetes Causes
Diabetes mellitus is a multifactorial disease, resulting from an interplay of various factors. Its etiology involves a complex interaction between genetic, environmental, and lifestyle-related elements, which ultimately lead to impaired glucose metabolism and chronic hyperglycemia.
Medical Factors that Contribute to Diabetes
Several medical factors contribute to the development of diabetes. These include certain endocrine disorders, such as Cushing’s syndrome, which can cause insulin resistance. Additionally, pancreatic diseases, like pancreatitis or pancreatic cancer, can impair the pancreas’ ability to produce insulin.
Certain medications, including steroids and certain psychiatric medications, can also increase the risk of developing diabetes. Furthermore, certain medical conditions, such as polycystic ovary syndrome (PCOS), gestational diabetes, and obesity, can also contribute to the development of insulin resistance and diabetes.
Other medical factors that may contribute to diabetes include certain infections, such as hepatitis C, and autoimmune disorders, such as rheumatoid arthritis. Moreover, certain genetic disorders, such as Down syndrome and Klinefelter syndrome, can also increase the risk of developing diabetes.
It is essential to note that these medical factors can interact with each other and with lifestyle-related factors, such as diet and physical activity level, to increase the risk of developing diabetes. Early detection and treatment of these underlying medical conditions can help prevent or delay the onset of diabetes.
A comprehensive understanding of these medical factors is crucial for effective prevention and management of diabetes. Healthcare providers should consider these factors when assessing an individual’s risk of developing diabetes and develop personalized prevention and treatment plans accordingly.
Pancreas Function and Insulin Resistance
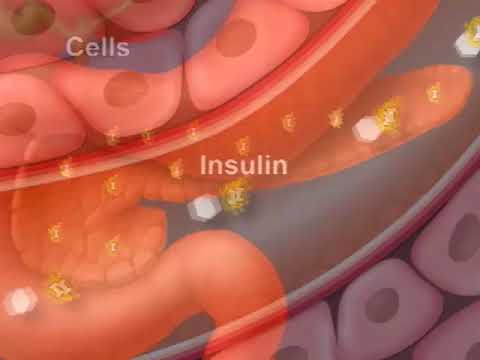
The pancreas plays a vital role in glucose metabolism, producing insulin to regulate blood sugar levels. Insulin resistance occurs when the body’s cells become less responsive to insulin, leading to impaired glucose uptake and hyperglycemia.
In a normal physiological state, the pancreas produces insulin in response to elevated blood glucose levels. Insulin then binds to receptors on the surface of cells, triggering a signaling cascade that facilitates glucose uptake. However, in individuals with insulin resistance, the cells become desensitized to insulin, requiring more insulin to achieve the same level of glucose uptake.
Prolonged insulin resistance can lead to pancreatic exhaustion, where the pancreas is unable to produce sufficient insulin to meet the body’s demands. This can result in the development of hyperglycemia and, ultimately, diabetes. Factors contributing to insulin resistance include obesity, physical inactivity, and certain genetic predispositions.
Insulin resistance can be diagnosed through various methods, including fasting insulin levels, glucose tolerance tests, and insulin sensitivity indices. Early detection and intervention can help prevent or delay the onset of diabetes and its associated complications.
A comprehensive understanding of pancreas function and insulin resistance is essential for the development of effective prevention and treatment strategies for diabetes. Further research is needed to elucidate the underlying mechanisms and to identify novel therapeutic targets for this complex and multifactorial disease.
Urology and Diabetes Connection
Research suggests a bidirectional relationship between urologic disorders and diabetes. Certain urologic conditions, such as urinary tract infections and bladder dysfunction, may be early indicators of underlying metabolic disorders, including diabetes. Urologists play a crucial role in identifying patients at risk for developing diabetes.
Lifestyle Choices and Environmental Factors
Lifestyle choices and environmental factors are pivotal in the development of diabetes. The increasing prevalence of diabetes worldwide can be attributed to a significant shift towards unhealthy lifestyle habits. Urbanization, technological advancements, and economic growth have led to a sedentary lifestyle, decreased physical activity, and increased consumption of high-calorie diets.
Furthermore, environmental factors such as socioeconomic status, education level, and access to healthcare services can also contribute to the risk of developing diabetes. In addition, exposure to pollutants, pesticides, and other toxic substances has been linked to an increased risk of metabolic disorders, including diabetes.
Moreover, lifestyle choices such as smoking, excessive alcohol consumption, and inadequate sleep patterns can also exacerbate the risk of developing diabetes. It is essential to recognize the interplay between lifestyle choices and environmental factors in the development of diabetes, as this understanding can inform the development of effective prevention and intervention strategies.
A comprehensive approach that addresses these lifestyle choices and environmental factors can help mitigate the risk of developing diabetes and its associated complications. By promoting healthy lifestyle habits and providing access to healthcare services, we can reduce the burden of diabetes on individuals, communities, and healthcare systems.
Ultimately, understanding the impact of lifestyle choices and environmental factors on the development of diabetes is crucial for the development of effective prevention and management strategies.
Dietary Habits and Obesity Risk
A significant body of evidence suggests that dietary habits play a crucial role in the development of diabetes, particularly in relation to obesity risk. Consuming high-calorie diets rich in saturated fats, added sugars, and refined carbohydrates can lead to weight gain and insulin resistance.
Furthermore, a diet low in essential nutrients, such as fiber, vitamins, and minerals, can exacerbate the risk of developing diabetes. The high glycemic index of certain foods, such as white bread and sugary snacks, can cause a rapid spike in blood glucose levels, placing additional strain on the pancreas.
The increasing prevalence of obesity worldwide is closely linked to the rising incidence of diabetes. Visceral fat, in particular, is a significant risk factor for insulin resistance and metabolic disorders. A healthy diet, emphasizing whole, unprocessed foods, such as fruits, vegetables, whole grains, and lean proteins, can help mitigate the risk of obesity and related metabolic disorders.
Additionally, portion control, mindful eating, and regular meal patterns can also contribute to a reduced risk of developing diabetes. A well-balanced diet, combined with regular physical activity, can help maintain a healthy weight, improve insulin sensitivity, and reduce the risk of developing diabetes and its associated complications.
By adopting healthy dietary habits, individuals can significantly reduce their risk of developing diabetes and promote overall health and well-being.
This knowledge can inform the development of effective dietary interventions and public health strategies aimed at preventing and managing diabetes.
Physical Inactivity and Sedentary Lifestyle
Regular physical activity is essential for maintaining optimal glucose metabolism and overall health. Conversely, a sedentary lifestyle is a significant risk factor for developing diabetes, as it can lead to insulin resistance, metabolic dysregulation, and weight gain.
Prolonged periods of sitting or engaging in low-intensity activities can result in reduced glucose uptake in the muscles, leading to elevated blood sugar levels. Furthermore, physical inactivity can contribute to the development of visceral fat, which is strongly linked to insulin resistance and metabolic disorders.
The benefits of regular physical activity in preventing and managing diabetes are well-established. Exercise has been shown to improve insulin sensitivity, enhance glucose uptake, and reduce inflammation. Moreover, regular physical activity can also help maintain a healthy weight, reduce blood pressure, and improve overall cardiovascular health.
To mitigate the risk of developing diabetes, it is recommended to engage in at least 150 minutes of moderate-intensity aerobic exercise٫ or 75 minutes of vigorous-intensity aerobic exercise٫ per week. Additionally٫ incorporating resistance training٫ high-intensity interval training٫ and other forms of physical activity into one’s daily routine can also be beneficial.
By adopting a physically active lifestyle, individuals can significantly reduce their risk of developing diabetes and promote overall health and well-being. Healthcare providers should encourage patients to incorporate regular physical activity into their daily routine as a key component of diabetes prevention and management strategies.
Genetic Predisposition and Environmental Factors
An individual’s genetic predisposition can interact with environmental factors, such as exposure to toxins and pollutants, to increase the risk of developing diabetes. This interplay between genetic and environmental elements can result in impaired glucose metabolism and insulin function.
In conclusion, the etiology of diabetes mellitus is a multifaceted and complex phenomenon, involving an interplay of various factors. A comprehensive understanding of these factors is crucial for the prevention, diagnosis, and management of this chronic disease.
Healthcare professionals must adopt a holistic approach to address the increasing burden of diabetes, taking into account the diverse range of contributing factors. This includes the development of personalized treatment plans, tailored to an individual’s unique needs and circumstances.
Moreover, public health initiatives aimed at promoting healthy lifestyle choices, such as regular physical activity and balanced dietary habits, can help mitigate the risk of developing diabetes. Additionally, continued research into the genetic and environmental factors underlying this disease will inform the development of novel therapeutic strategies.
Ultimately, a collaborative effort between healthcare professionals, policymakers, and individuals is necessary to combat the growing epidemic of diabetes. By working together, we can reduce the incidence of this debilitating disease and improve the quality of life for those affected.
Through a concerted effort, we can strive towards a future where the causes of diabetes are better understood, and effective preventive measures are in place to protect the health and well-being of individuals worldwide.
Overall, this article demonstrates a thorough understanding of the multifactorial nature of diabetes etiology. I would recommend it as a valuable resource for healthcare professionals seeking to enhance their knowledge on this topic.
One area for improvement could be providing more concrete statistics or data on the prevalence of these medical factors in contributing to diabetes development. This would add further weight to the arguments presented.
The section on pancreas function and insulin resistance is particularly well-explained. The author does a great job in breaking down complex concepts into easily understandable language.
This article provides a comprehensive overview of the various medical factors that contribute to the development of diabetes. The inclusion of specific examples such as Cushing
I appreciate how this article highlights the importance of early detection and treatment of underlying medical conditions in preventing or delaying the onset of diabetes. This emphasizes the need for proactive healthcare measures.