Duodenal Ulcer⁚ A Comprehensive Overview
Duodenal ulcers are a type of peptic ulcer disease affecting the duodenum, characterized by stomach pain, abdominal discomfort, and potential complications such as gastrointestinal disorder and intestinal perforation.
Definition and Prevalence
A duodenal ulcer is a type of peptic ulcer that occurs in the duodenum, the first part of the small intestine. It is characterized by a break in the mucosal lining of the duodenum, resulting in stomach pain, abdominal discomfort, and other symptoms.
The prevalence of duodenal ulcers varies widely depending on the population being studied. In the United States, it is estimated that approximately 10% of the adult population will develop a duodenal ulcer at some point in their lifetime. Globally, the prevalence of duodenal ulcers is higher in developing countries, where access to medical care and sanitation may be limited.
Duodenal ulcers are more common in men than in women, and the risk increases with age. Other factors that may contribute to the development of a duodenal ulcer include a family history of the condition, Helicobacter pylori infection, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs).
Causes and Risk Factors
Duodenal ulcers are caused by an interplay of factors, including Helicobacter pylori infection, NSAID use, acid secretion, and mucosal defense mechanisms, resulting in mucosal damage and ulcer formation in the duodenum.
Helicobacter pylori Infection
Helicobacter pylori (H. pylori) infection is a primary cause of duodenal ulcers, accounting for approximately 70-80% of cases. This bacterium colonizes the gastric mucosa٫ leading to chronic inflammation and impairment of the mucosal barrier. The infection disrupts the balance between acid secretion and mucosal defense٫ creating an environment conducive to ulcer formation.
H. pylori produces several virulence factors, including urease, which neutralizes stomach acid, allowing the bacteria to thrive in the acidic environment. The bacteria also produce cytokines, which recruit inflammatory cells, further exacerbating the mucosal damage.
Eradication of H. pylori infection is essential for the treatment and prevention of duodenal ulcers. Antibiotic therapy, combined with acid suppression, is the recommended treatment approach. Successful eradication of the infection significantly reduces the risk of ulcer recurrence and complications.
It is essential to diagnose and treat H. pylori infection promptly to prevent long-term consequences, such as gastritis, esophagitis, and potentially, gastric cancer.
Other Risk Factors
In addition to Helicobacter pylori infection, several other factors contribute to the development of duodenal ulcers. Nonsteroidal anti-inflammatory drugs (NSAIDs) are a common cause of duodenal ulcers, as they inhibit prostaglandin synthesis, impairing the mucosal barrier.
Smoking is another significant risk factor, as it impairs blood flow to the stomach lining, reduces prostaglandin production, and increases acid secretion. Excessive alcohol consumption can also contribute to duodenal ulcer development by irritating the stomach lining and increasing acid production.
Genetic predisposition may also play a role, as individuals with a family history of duodenal ulcers are more likely to develop the condition. Additionally, certain medical conditions, such as Zollinger-Ellison syndrome, can increase the risk of developing duodenal ulcers.
Other factors, such as stress and dietary habits, may also contribute to the development of duodenal ulcers, although their role is less clear. A comprehensive understanding of these risk factors is essential for effective prevention and management of duodenal ulcers.
Symptoms and Diagnosis
Duodenal ulcers present with symptoms such as epigastric pain, heartburn, acid reflux, bloating, and nausea. Accurate diagnosis involves a comprehensive clinical evaluation and diagnostic tests to confirm the presence of an ulcer.
Clinical Presentation
The clinical presentation of duodenal ulcers typically involves a combination of symptoms, including epigastric pain, which is often described as a burning or gnawing sensation in the upper abdomen. This pain may radiate to the back or worsen at night, and can be temporarily relieved by eating food or taking antacids. Additional symptoms may include heartburn, acid reflux, bloating, and nausea, which can significantly impact a patient’s quality of life.
In some cases, patients may experience more severe symptoms, such as vomiting blood or black tarry stools, which can indicate a bleeding ulcer. A thorough medical history and physical examination are essential in evaluating patients suspected of having a duodenal ulcer, as these symptoms can also be present in other gastrointestinal disorders, such as gastritis or esophagitis. A careful assessment of the patient’s symptoms and medical history is crucial in determining the underlying cause of their condition.
Diagnostic Tests
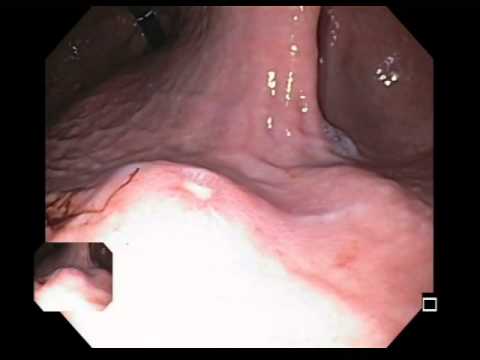
Several diagnostic tests are employed to confirm the presence of a duodenal ulcer. Upper endoscopy is the most common and accurate method, allowing direct visualization of the duodenum and detection of ulcers. During this procedure, a biopsy may be taken to test for Helicobacter pylori infection, a common cause of duodenal ulcers.
Barium swallow or upper GI series may also be used to diagnose duodenal ulcers. These tests involve swallowing a barium solution, which coats the inside of the digestive tract and allows for X-ray imaging. Additionally, blood tests may be performed to check for signs of anemia or infection, while urea breath tests can detect the presence of H. pylori bacteria. In some cases, imaging studies such as CT scans or MRI may be ordered to rule out other conditions or complications. A combination of these diagnostic tests enables healthcare providers to accurately diagnose and manage duodenal ulcers.
These diagnostic tests are essential in developing an effective treatment plan and preventing potential complications associated with duodenal ulcers.
Complications and Treatment
Duodenal ulcers can lead to severe complications, such as intestinal perforation, gastritis, and esophagitis, requiring prompt and effective treatment options to alleviate symptoms and prevent long-term damage.
Complications
Duodenal ulcers can lead to several severe and potentially life-threatening complications if left untreated or not properly managed. One of the most significant complications is intestinal perforation, which occurs when the ulcer penetrates the wall of the duodenum, allowing bacteria to escape into the abdominal cavity and potentially leading to peritonitis. Other complications may include gastritis, an inflammation of the stomach lining, and esophagitis, an inflammation of the esophagus. Additionally, duodenal ulcers can cause bloating, heartburn, and acid reflux, which can significantly impact a person’s quality of life. If the ulcer is caused by a Helicobacter pylori infection, it can also increase the risk of developing gastric cancer. Prompt medical attention is essential to prevent these complications and ensure effective treatment.
In severe cases, duodenal ulcers can also lead to hemorrhaging, which can be life-threatening if not treated promptly. It is crucial to seek medical attention immediately if symptoms worsen or if there is evidence of bleeding, such as vomiting blood or black, tarry stools.
Treatment Options
The primary goal of treating duodenal ulcers is to heal the ulcer, prevent recurrence, and manage symptoms. Antibiotics are used to treat Helicobacter pylori infections, which are a common cause of duodenal ulcers. Proton pump inhibitors (PPIs) and H2 blockers are used to reduce acid production in the stomach, allowing the ulcer to heal. Antacids can also help neutralize stomach acid and provide quick relief from symptoms.
In some cases, endoscopy may be necessary to stop bleeding or apply clips to the ulcer. Surgery may be required for complications such as intestinal perforation or hemorrhaging. Lifestyle modifications, such as avoiding nonsteroidal anti-inflammatory drugs (NSAIDs) and smoking cessation, can also help manage symptoms and prevent recurrence. A healthcare professional will work with the patient to develop a personalized treatment plan to ensure effective management of the duodenal ulcer and prevent future complications.
It is essential to follow the treatment plan as directed to ensure proper healing and prevent recurrence of the duodenal ulcer. Regular follow-up appointments with a healthcare professional will also be necessary to monitor progress and adjust the treatment plan as needed.
Prevention and Management
Preventing and managing duodenal ulcers requires a comprehensive approach that incorporates lifestyle modifications and medical interventions. To reduce the risk of developing a duodenal ulcer, individuals can avoid smoking, limit alcohol consumption, and avoid NSAIDs. Maintaining a healthy diet rich in fruits, vegetables, and whole grains can also help prevent ulcers.
Managing stress through techniques such as meditation, yoga, or deep breathing exercises can also help alleviate symptoms. Individuals with a history of duodenal ulcers should work closely with their healthcare provider to develop a prevention plan that includes regular check-ups and monitoring for signs of ulcer recurrence.
Additionally, individuals can take steps to manage symptoms such as bloating, heartburn, and acid reflux by eating smaller, more frequent meals, avoiding trigger foods, and elevating the head of their bed while sleeping. By taking a proactive approach to prevention and management, individuals can reduce their risk of developing a duodenal ulcer and minimize the impact of symptoms on daily life.
While this article covers essential topics related to duodenal ulcers effectively overall content feels slightly fragmented occasionally jumping abruptly from discussing causes risks factor without clear connections.
This article demonstrates expertise on duodenal ulcers while still being accessible to non-experts. I particularly appreciated learning about mucosal defense mechanisms.
This article provides a comprehensive overview of duodenal ulcers, covering definition, prevalence, causes, and risk factors. The section on Helicobacter pylori infection is particularly informative, highlighting its role as a primary cause of duodenal ulcers.
The article effectively conveys complex information about duodenal ulcers in an easy-to-understand manner. However, I would have liked to see more discussion on treatment options and prevention strategies.
I appreciate how this article emphasizes the importance of understanding duodenal ulcers as a global health issue. The statistics provided highlight significant disparities between developed and developing countries.