Introduction to Epididymitis
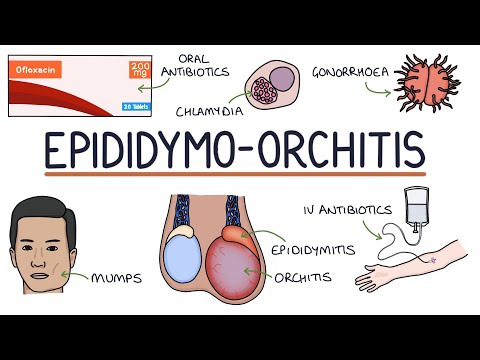
Epididymitis is a condition characterized by inflammation of the epididymis, a tube-like structure storing sperm behind each testicle. It affects male reproductive health, often caused by bacterial infections, and requires prompt medical attention to prevent long-term complications.
Causes and Risk Factors
Epididymitis is typically caused by bacterial infections, often resulting from urinary tract infections or sexually transmitted diseases. Risk factors include recent urinary tract instrumentation, unprotected sex, and pre-existing urological conditions, increasing susceptibility to infection.
Bacterial Infections
Bacterial infections are the primary cause of epididymitis, with the most common pathogens being Chlamydia trachomatis, Neisseria gonorrhoeae, and gram-negative bacilli. These bacteria can ascend from the urethra or prostate, causing inflammation and infection in the epididymis.
In sexually active men, Chlamydia trachomatis is the most common cause of epididymitis, while in older men, bacterial urinary tract infections are more likely to be the cause. The bacteria can also be introduced through instrumentation, such as catheterization or cystoscopy.
The risk of bacterial epididymitis is increased in men with pre-existing urological conditions, such as benign prostatic hyperplasia or urinary tract obstruction. Unprotected sex and a history of sexually transmitted diseases also increase the risk of developing bacterial epididymitis.
Prompt antibiotic treatment is essential to manage bacterial epididymitis and prevent long-term complications, such as infertility and chronic pain. A comprehensive medical evaluation, including urine cultures and imaging studies, may be necessary to determine the underlying cause of the infection.
Other Causes
In addition to bacterial infections, other causes of epididymitis include non-bacterial pathogens, such as viruses and fungi. Viral epididymitis is often associated with mumps orchitis, while fungal epididymitis is more common in immunocompromised individuals.
Trauma to the scrotum or epididymis can also cause inflammation and lead to epididymitis. This type of trauma may be due to a direct blow to the scrotum or from activities that cause repetitive strain on the epididymis, such as heavy lifting or strenuous exercise.
Certain medications, such as amiodarone, can cause epididymitis as a side effect. Additionally, underlying medical conditions, like Behçet’s disease or granulomatosis with polyangiitis, can increase the risk of developing epididymitis.
Rarely, epididymitis can be caused by obstructive factors, such as urethral stricture or ejaculatory duct obstruction. In some cases, the cause of epididymitis may remain unknown, highlighting the importance of a comprehensive medical evaluation to determine the underlying cause of the condition.
A thorough understanding of the various causes of epididymitis is essential for effective diagnosis and management of the condition.
Symptoms of Epididymitis
Epididymitis presents with a range of symptoms affecting the male reproductive system, including pain, swelling, and inflammation. Common signs include scrotal tenderness, abnormal seminal discharge, and urinary disturbances, necessitating prompt medical evaluation and treatment.
Pain and Swelling
The primary symptoms of epididymitis are pain and swelling in the affected testicle, often accompanied by redness and warmth of the scrotal skin. This pain can range from mild to severe and may radiate to the groin or lower abdomen. The swelling is usually unilateral, affecting one testicle, but in some cases, it can be bilateral.
Patients may experience tenderness upon palpation of the affected testicle, and the scrotum may become enlarged due to the accumulation of fluid, a condition known as hydrocele. The pain and swelling associated with epididymitis can worsen over time if left untreated, potentially leading to more severe complications.
In addition to these local symptoms, some patients may experience referred pain in the groin or lower back, which can be exacerbated by physical activity or straining. It is essential to seek medical attention promptly if experiencing persistent or severe pain and swelling in the testicles, as timely treatment can help alleviate symptoms and prevent long-term damage.
Urinary Symptoms
In addition to pain and swelling, epididymitis can cause a range of urinary symptoms. Patients may experience painful urination, also known as dysuria, which can be accompanied by a burning sensation or discomfort while urinating.
Some individuals may notice an abnormal discharge from the penis, which can be cloudy, yellowish, or greenish in color. This discharge may be foul-smelling and can be a sign of an underlying infection. Hematuria, or blood in the urine, is another possible symptom of epididymitis.
Urinary frequency or urgency can also occur, leading to an increased need to urinate throughout the day. Nocturia, or frequent nighttime urination, may disrupt sleep patterns and contribute to overall discomfort. It is essential to seek medical attention if experiencing any unusual urinary symptoms, as these can indicate an underlying condition that requires prompt treatment.
A healthcare professional will evaluate these urinary symptoms in conjunction with other diagnostic factors to determine the underlying cause of epididymitis and develop an effective treatment plan.
Complications of Untreated Epididymitis
Untreated epididymitis can lead to severe complications, including chronic pain, infertility, and scrotal swelling. Prompt medical attention is essential to prevent long-term damage to the reproductive system and mitigate potential future health issues.
Fertility Issues
One of the most significant complications of untreated epididymitis is fertility issues. The inflammation and scarring caused by the infection can damage the delicate tubes and structures within the epididymis, leading to impaired sperm function and reduced fertility.
In some cases, the infection can cause a complete blockage of the epididymal tube, preventing sperm from being released during ejaculation. This can result in azoospermia, a condition characterized by the absence of sperm in the semen.
The likelihood of fertility issues due to epididymitis depends on the severity and duration of the infection. Mild cases may not have a significant impact on fertility, while more severe cases can lead to permanent damage. It is essential for individuals experiencing symptoms of epididymitis to seek medical attention promptly to minimize the risk of long-term fertility issues.
Early treatment can help alleviate symptoms, reduce inflammation, and prevent scarring, thereby preserving fertility. However, in some cases, fertility treatments such as assisted reproductive technology (ART) may be necessary to achieve conception.
Chronic Pain and Inflammation
Untreated epididymitis can lead to chronic pain and inflammation in the affected testicle and surrounding areas. This can result in persistent discomfort, tenderness, and swelling, significantly impacting an individual’s quality of life.
Chronic epididymitis can cause recurring episodes of pain, which can be exacerbated by physical activity, sexual intercourse, or even simple movements. In some cases, the pain can be severe enough to interfere with daily activities and sleep patterns.
The chronic inflammation associated with untreated epididymitis can also lead to the formation of scar tissue, adhesions, and calcifications within the epididymis. These complications can further contribute to chronic pain and discomfort.
It is essential for individuals experiencing chronic pain and inflammation due to epididymitis to seek medical attention. A healthcare professional can develop a treatment plan to manage symptoms, reduce inflammation, and prevent long-term complications. This may include pain management strategies, anti-inflammatory medications, and lifestyle modifications to alleviate discomfort and promote healing.
Diagnosis and Treatment Options
Accurate diagnosis of epididymitis involves medical evaluation, physical examination, and diagnostic testing. Treatment options typically include antibiotics to address underlying infections, pain management strategies, and supportive care to alleviate symptoms and promote recovery.
Medical Evaluation and Testing
A comprehensive medical evaluation is essential for diagnosing epididymitis. A healthcare professional will conduct a thorough physical examination to assess the affected area, checking for signs of swelling, tenderness, and redness. A medical history will also be taken to identify potential underlying causes and risk factors.
Diagnostic testing may include⁚
- Urinalysis to detect the presence of bacteria or other abnormalities in the urine
- Urine cultures to identify the specific type of bacteria causing the infection
- Blood tests to rule out other conditions that may cause similar symptoms
- Imaging studies, such as ultrasound or CT scans, to visualize the affected area and assess for complications
A diagnosis of epididymitis is typically made based on a combination of clinical findings, medical history, and diagnostic test results. A healthcare professional will use this information to develop an effective treatment plan and manage symptoms.
Antibiotic Treatment and Pain Management
Antibiotics are the primary treatment for bacterial epididymitis. The type and duration of antibiotic therapy will depend on the severity of the infection, the type of bacteria causing the infection, and the individual’s overall health.
Common antibiotics used to treat epididymitis include⁚
- Doxycycline
- Ceftriaxone
- Ciprofloxacin
In addition to antibiotic therapy, pain management is also crucial in treating epididymitis. Over-the-counter pain medications, such as acetaminophen or ibuprofen, may be prescribed to help alleviate discomfort and reduce inflammation. In some cases, stronger pain medications may be necessary.
Bed rest, applying ice packs to the affected area, and elevating the scrotum can also help manage symptoms and promote recovery. It is essential to complete the full course of antibiotic treatment as directed by a healthcare professional to ensure effective treatment and prevent complications.
Prevention and Self-Care
Preventing epididymitis requires a combination of safe sex practices, good hygiene, and maintaining overall health. To reduce the risk of infection⁚
- Practice safe sex using condoms to prevent the transmission of STIs.
- Avoid unprotected sex with multiple partners.
- Urinate after intercourse to help flush out bacteria from the urethra.
Maintaining good genital hygiene is also crucial. This includes⁚
- Washing the genital area regularly with mild soap and water.
- Avoiding tight-fitting clothing that can irritate the scrotum.
- Wearing breathable underwear to help keep the genital area dry.
Regular check-ups with a healthcare provider can also help identify any underlying conditions that may increase the risk of epididymitis. By taking these preventative measures, individuals can significantly reduce their risk of developing epididymitis and maintain optimal male reproductive health.
I would have liked to see more information on prevention strategies for reducing the risk of developing epididymitis.
This article is well-written and easy to understand for non-medical professionals.
The article could benefit from more information on non-bacterial causes of epididymitis, such as viral and fungal infections.
This article provides a comprehensive overview of epididymitis, including its causes, risk factors, and treatment options. The section on bacterial infections is particularly informative.
Overall, this article provides a clear understanding of epidemicitymitis; however minor formatting adjustments could enhance readability.
As a healthcare professional, I appreciate the accuracy and detail provided in this article about epididymitis.
I appreciate how this article highlights the importance of prompt medical attention in preventing long-term complications from epididymitis.
The section on risk factors could be expanded to include more specific examples.