Introduction to Epigastric Hernia in Adults
Epigastric hernia in adults is a significant health concern, requiring prompt attention and treatment to prevent complications. Occurring in the epigastric region, it necessitates comprehensive understanding for effective management.
1.1 Definition and Prevalence of Epigastric Hernia
Epigastric hernia is defined as a protrusion of abdominal contents through a defect in the abdominal wall, specifically in the epigastric region, which is located between the xiphoid process and the umbilicus. This type of hernia is relatively common in adults, accounting for approximately 1-5% of all hernia cases.
The prevalence of epigastric hernia varies depending on factors such as age, sex, and body mass index (BMI). Studies have shown that epigastric hernia is more common in men than in women, with a male-to-female ratio of approximately 3⁚1. Additionally٫ the prevalence of epigastric hernia increases with age٫ with the majority of cases occurring in individuals over the age of 40.
The exact incidence of epigastric hernia is difficult to determine, as many cases may be asymptomatic or misdiagnosed. However, it is estimated that approximately 10-20% of adults will develop an epigastric hernia at some point in their lifetime.
Causes and Risk Factors of Epigastric Hernia
Epigastric hernia in adults is multifactorial, resulting from a combination of genetic predisposition, acquired weaknesses in the abdominal wall, and increased intra-abdominal pressure, ultimately leading to herniation.
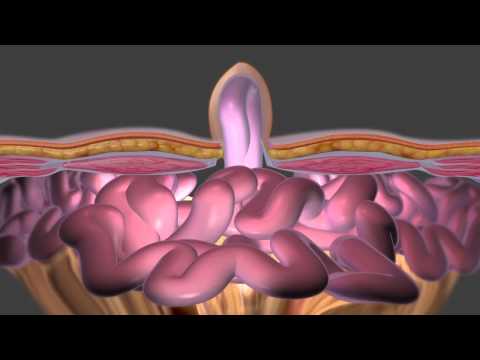
2.1 Abdominal Wall Defects and Stomach Protrusion
Abdominal wall defects are a primary cause of epigastric hernia in adults, allowing the stomach to protrude through the weakened area. This occurs when the abdominal wall, comprising muscles and tendons, is compromised due to various factors such as congenital conditions, trauma, or surgical incisions. As a result, the stomach, which is normally confined within the abdominal cavity, bulges outward, creating a visible lump or swelling in the epigastric region.
The protrusion of the stomach can lead to discomfort, pain, and potentially life-threatening complications if left untreated. The abdominal wall defect can be attributed to a weakening of the transversalis fascia, a layer of tissue that provides support to the abdominal wall. When this fascia is compromised, it can no longer maintain the integrity of the abdominal wall, allowing the stomach to herniate through the weakened area.
A thorough understanding of abdominal wall defects and stomach protrusion is essential for the diagnosis and treatment of epigastric hernia in adults.
2.2 Diaphragm Weakness and Upper Abdominal Pain
Diaphragm weakness is a significant contributing factor to epigastric hernia in adults, often manifesting as upper abdominal pain. The diaphragm, a dome-shaped muscle separating the chest and abdominal cavities, plays a crucial role in maintaining intra-abdominal pressure. When the diaphragm is weakened, it can no longer effectively regulate this pressure, leading to increased stress on the abdominal wall.
This increased stress can cause the abdominal wall to bulge, resulting in an epigastric hernia. Upper abdominal pain is a common symptom of diaphragm weakness, as the herniated stomach can irritate surrounding tissues and nerves. Patients may experience sharp, stabbing pains or dull, aching sensations in the upper abdomen, which can worsen with coughing, lifting, or straining.
A weak diaphragm can also contribute to breathing difficulties and decreased lung capacity, further complicating the clinical presentation of epigastric hernia. A comprehensive evaluation of diaphragm function is essential for accurate diagnosis and effective treatment of epigastric hernia in adults;
Symptoms and Diagnosis of Epigastric Hernia
Accurate diagnosis of epigastric hernia relies on a thorough evaluation of symptoms, medical history, and physical examination, supplemented by diagnostic tests to confirm the presence and extent of the hernia.
3.1 Hernia Symptoms and Midline Hernias
Epigastric hernia symptoms in adults can vary in severity and presentation. Typically, patients experience discomfort or pain in the upper abdominal region, which may worsen with coughing, straining, or heavy lifting. A visible bulge or protrusion may be noticeable, especially when standing upright. Midline hernias, occurring near the navel, can be tender to the touch and may be accompanied by a feeling of heaviness or dragging sensation. In some cases, hernia symptoms may be absent or mild, making diagnosis more challenging. A thorough physical examination and medical history are essential to identify potential hernias and determine the need for further evaluation. Symptoms can also be exacerbated by factors such as obesity, constipation, or chronic coughing, emphasizing the importance of a comprehensive assessment to accurately diagnose epigastric hernia in adults.
3;2 Diagnostic Tests and Procedures
Accurate diagnosis of epigastric hernia in adults involves a combination of physical examination, imaging studies, and endoscopic procedures. Initially, a thorough physical examination is performed to assess the abdominal wall and identify potential hernias. Imaging tests, such as ultrasound, computed tomography (CT) scans, or magnetic resonance imaging (MRI), may be ordered to confirm the presence of a hernia and evaluate its size and location. Endoscopic procedures, including upper endoscopy or laparoscopy, may be used to visualize the hernia and assess for potential complications. In some cases, a barium swallow or upper gastrointestinal series may be performed to evaluate the digestive tract and rule out other conditions. A comprehensive diagnostic approach ensures accurate identification of epigastric hernia in adults, enabling effective treatment planning and minimizing the risk of complications.
Treatment Options for Epigastric Hernia
Treatment options for epigastric hernia in adults vary depending on the severity and size of the hernia. A multidisciplinary approach, including surgical and non-surgical interventions, aims to alleviate symptoms and prevent complications.
4.1 Surgical Repair of Epigastric Hernia
Surgical repair of epigastric hernia is a common treatment approach, often recommended for symptomatic hernias or those at risk of complications. The primary goal of surgery is to restore the integrity of the abdominal wall, prevent further herniation, and alleviate symptoms. Surgical techniques may vary depending on the size and location of the hernia, as well as the patient’s overall health status. In general, surgical repair involves the closure of the hernia defect using sutures, mesh, or a combination of both. Laparoscopic and open repair techniques are available, each with its own benefits and risks. A thorough evaluation by a qualified surgeon is essential to determine the most suitable surgical approach for each individual patient. Postoperative care and follow-up are crucial to ensure optimal outcomes and minimize the risk of complications.
4.2 Non-Surgical Treatment Options
Non-surgical treatment options for epigastric hernia in adults are typically reserved for asymptomatic or mildly symptomatic hernias. A watchful waiting approach may be adopted, with regular monitoring to assess for potential complications or worsening symptoms. Lifestyle modifications, such as weight loss, dietary changes, and stress reduction, may also be recommended to alleviate symptoms and reduce the risk of complications. Additionally, supportive garments or binders may be prescribed to provide temporary relief from discomfort and help manage symptoms. It is essential for patients to work closely with their healthcare provider to determine the most suitable non-surgical treatment plan and schedule regular follow-up appointments to monitor the hernia’s progression. Furthermore, patients should be aware of the potential risks and limitations associated with non-surgical treatment and be prepared to consider surgical intervention if their condition worsens or complications arise.
Complications and Adult Health Issues
Untreated epigastric hernia in adults can lead to severe complications, impacting overall health and quality of life. Prompt recognition and management of these complications are crucial to prevent long-term consequences and optimize patient outcomes.
5.1 Complications of Untreated Epigastric Hernia
Untreated epigastric hernia in adults can lead to several complications, including incarceration, strangulation, and obstruction of the herniated contents. These complications can result in severe abdominal pain, nausea, vomiting, and potentially life-threatening conditions, such as peritonitis and sepsis.
Incarceration occurs when the herniated contents become trapped, leading to bowel obstruction, while strangulation occurs when the blood supply to the herniated contents is compromised, resulting in tissue necrosis. Furthermore, untreated epigastric hernia can also lead to chronic health issues, such as gastroesophageal reflux disease (GERD), dysphagia, and malnutrition.
Prompt recognition and treatment of these complications are essential to prevent long-term consequences and optimize patient outcomes. A thorough understanding of the potential complications of untreated epigastric hernia is crucial for healthcare professionals to provide effective management and care for affected individuals.
In addition, early intervention and treatment can significantly reduce the risk of these complications and improve the overall quality of life for individuals with epigastric hernia.
5.2 Prevention and Management of Epigastric Hernia
Prevention and management of epigastric hernia in adults involve a multifaceted approach, including lifestyle modifications, dietary changes, and post-operative care. Maintaining a healthy weight, avoiding heavy lifting, and managing stress can help reduce the risk of hernia recurrence.
A balanced diet rich in fiber, fruits, and vegetables can help prevent constipation and reduce abdominal strain. Additionally, avoiding foods that trigger acid reflux and heartburn can help alleviate symptoms associated with epigastric hernia.
Post-operative care is crucial to prevent complications and promote healing. Patients should follow a structured recovery plan, including pain management, wound care, and follow-up appointments with their healthcare provider.
Moreover, patients should be educated on recognizing signs of hernia recurrence and complications, such as abdominal pain, nausea, and vomiting. By adopting a proactive approach, individuals can effectively manage their condition and minimize the risk of long-term complications.
Regular monitoring and follow-up care can significantly improve patient outcomes and quality of life.
This article provides a comprehensive overview of epigastric hernias in adults, including their definition, prevalence, causes, and risk factors.
The section on causes and risk factors is particularly informative; however, I would like to see more discussion on potential preventive measures.
“The formatting makes reading easy but incorporating visual aids could improve comprehension.”
I appreciate how this article highlights the importance of prompt attention and treatment for epigastric hernias to prevent complications.
I found this article well-written; though I believe incorporating case studies could enhance reader engagement.
This article effectively communicates complex medical information; yet there could be further explanation on differences between types of abdominal wall defects.
The statistics provided on prevalence are interesting; however; I think it would be beneficial to include more data on outcomes following treatment.