Introduction to Leprosy
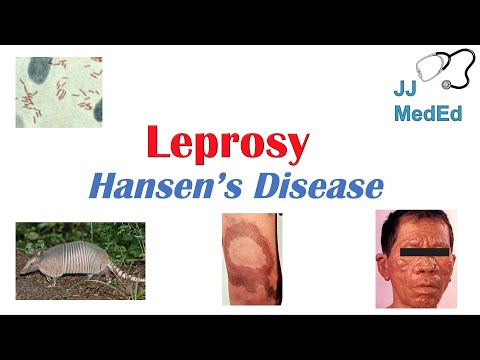
Leprosy, also known as Hansen’s disease, is a chronic bacterial infection caused by Mycobacterium leprae. With a long history of human suffering, leprosy remains a significant public health concern in many parts of the world, particularly in tropical and subtropical regions.
What is Leprosy?
Leprosy is a complex, multifaceted disease characterized by various clinical manifestations, ranging from mild skin lesions to severe nerve damage, resulting in physical disability and social stigma, posing a significant challenge to healthcare systems worldwide, particularly in resource-poor settings.
2.1 Definition and Causes
Leprosy, also known as Hansen’s disease, is a chronic bacterial infection caused by Mycobacterium leprae, primarily affecting the skin, peripheral nerves, mucosa of the upper respiratory tract, and the eyes. The bacteria are acid-fast, Gram-positive, and have a unique characteristic of infecting cooler parts of the human body, such as the skin and peripheral nerves.
The exact mechanism of leprosy transmission remains unclear; however, it is believed to occur through close and prolonged contact with an infected individual, particularly those with untreated multibacillary leprosy. Droplets from the nose and mouth of infected individuals may also play a role in transmission.
Mycobacterium leprae is thought to be spread through respiratory droplets that enter the body through the mucous membranes of the eyes, nose, or throat. Once inside the body, the bacteria begin to multiply, leading to damage to the skin, nerves, and other tissues, ultimately causing the characteristic symptoms of leprosy.
Understanding the definition and causes of leprosy is essential for developing effective strategies to prevent and control the spread of the disease, particularly in high-risk populations and endemic areas.
2.2 Leprosy Symptoms
The symptoms of leprosy can vary widely depending on the severity of the infection and the individual’s immune response. Early signs of leprosy may include skin lesions or rashes, which can be lighter or darker than the surrounding skin, as well as numbness or loss of sensation in the affected areas.
In more advanced cases, leprosy can cause significant nerve damage, leading to muscle weakness, paralysis, and disability. If left untreated, leprosy can also cause disfigurement and disability, including claw hand, foot ulcers, and vision loss.
Other common symptoms of leprosy include⁚
- Enlarged lymph nodes
- Fever
- Joint pain and swelling
- Nosebleeds and stuffiness
- Skin nodules or lumps
It is essential to note that leprosy symptoms can take years to develop, and in some cases, the disease may progress slowly over many years. Prompt medical attention is crucial for preventing long-term damage and disability associated with leprosy.
A thorough understanding of leprosy symptoms is vital for early diagnosis and treatment, which can significantly improve patient outcomes and prevent the spread of the disease.
Transmission Methods
Leprosy is primarily spread through the respiratory route, where an infected person releases droplets containing Mycobacterium leprae into the air, which can be inhaled by others.
Close and prolonged contact with an untreated individual is necessary for transmission to occur, typically through⁚
- Respiratory droplets⁚ coughing or sneezing
- Close living conditions⁚ households, dormitories, or other confined spaces
- Infected person’s skin lesions or rashes⁚ direct contact
- Contaminated water⁚ in rare cases, through contact with contaminated water sources
While leprosy is contagious, it has a relatively low transmission rate compared to other infectious diseases. The risk of transmission is higher among⁚
People living in close proximity to an untreated individual, such as family members or healthcare workers.
Individuals with weakened immune systems, such as those with chronic illnesses or malnutrition.
Children under the age of 15, who are more susceptible to infection due to their developing immune system.
Understanding transmission methods is crucial for implementing effective prevention and control measures to reduce the spread of leprosy.
Leprosy Symptoms and Diagnosis
Accurate diagnosis of leprosy involves a combination of clinical examination, bacteriological and pathological investigations, and consideration of the patient’s medical history, to identify characteristic skin lesions, nerve damage, and other indicative symptoms of Mycobacterium leprae infection.
4.1 Early Warning Signs
Early detection of leprosy is crucial to prevent long-term damage and disability. The initial symptoms can be subtle and may not always be immediately apparent. Typical early warning signs include⁚
- Skin lesions or rashes⁚ Discolored, numb, or tender patches on the skin, which can be lighter or darker than the surrounding skin.
- Numbness or loss of sensation⁚ Reduced or absent sensation in the skin, particularly in the extremities, such as hands and feet.
- Nerve pain or tingling⁚ Pain, tingling, or burning sensations in the nerves, often accompanied by weakness or paralysis of the affected area.
- Eye problems⁚ Dryness, redness, or vision loss due to corneal ulcers or other ocular complications.
- Muscle weakness⁚ Decreased muscle strength or paralysis, particularly in the face, arms, or legs.
If left untreated, these early warning signs can progress to more severe symptoms, leading to permanent nerve damage, disfigurement, and disability. It is essential to seek medical attention promptly if any of these symptoms are experienced, especially in regions where leprosy is prevalent.
4.2 Diagnostic Tests
A definitive diagnosis of leprosy is typically made through a combination of clinical examination, laboratory tests, and histopathological analysis.
The following diagnostic tests may be employed⁚
- Skin smears⁚ A sample of tissue is taken from the affected skin area and examined under a microscope for the presence of acid-fast bacilli (AFB).
- Skin biopsies⁚ A tissue sample is removed and examined for histopathological changes characteristic of leprosy, such as inflammation and nerve damage.
- Blood tests⁚ Serological tests can detect antibodies against Mycobacterium leprae, but these tests are not always reliable and may produce false-negative results.
- Nerve conduction studies⁚ These tests assess nerve function and can help diagnose nerve damage associated with leprosy.
It is essential to note that a single test may not be sufficient for a definitive diagnosis, and a combination of tests may be necessary to confirm the presence of leprosy. Furthermore, early diagnosis and treatment are critical to prevent long-term damage and disability.
A healthcare professional should be consulted for an accurate diagnosis and appropriate treatment plan.
Treatment Options
Leprosy is typically treated with antibiotics, which can effectively cure the disease and prevent long-term damage.
The primary treatment regimen for leprosy is multidrug therapy (MDT), which combines the following antibiotics⁚
- Dapsone⁚ A sulfone antibiotic that inhibits the growth of Mycobacterium leprae.
- Clofazimine⁚ An antimicrobial agent that has anti-inflammatory properties.
- Rifampicin⁚ A potent bactericidal antibiotic that kills Mycobacterium leprae.
The duration of treatment varies depending on the severity of the disease, but typically ranges from 6 to 12 months for paucibacillary leprosy and 12 to 24 months for multibacillary leprosy.
It is essential to complete the full course of treatment to ensure a cure and prevent the development of antibiotic resistance. In some cases, additional medications may be prescribed to manage symptoms and prevent complications.
Early treatment can significantly improve outcomes and reduce the risk of disability. A healthcare professional should be consulted to determine the best course of treatment for individual cases of leprosy.
With proper treatment, people with leprosy can lead active and fulfilling lives.
Complications and Prevention
Untreated leprosy can lead to significant complications, including permanent nerve damage, disfigurement, and disability.
Prevention of complications relies on early detection and treatment of the disease. Additionally, preventative measures can be taken to reduce the risk of transmission⁚
- Vaccination⁚ The BCG vaccine has been shown to offer some protection against leprosy.
- Contact tracing⁚ Identifying and screening individuals who have come into close contact with someone with leprosy can help prevent transmission.
- Improved hygiene⁚ Practicing good hygiene, such as washing hands regularly, can reduce the risk of transmission.
- Avoiding close contact⁚ Avoiding close contact with someone who has untreated leprosy can also reduce the risk of transmission.
In communities where leprosy is common, education and awareness campaigns can help promote early detection and treatment. Furthermore, addressing poverty, malnutrition, and inequality can also contribute to reducing the incidence of leprosy.
By taking a proactive approach to prevention and early detection, it is possible to reduce the impact of leprosy and prevent long-term complications.
Efforts to control and eliminate leprosy as a public health problem continue, with ongoing research into new treatments and vaccines.
This article provides a comprehensive introduction to leprosy, covering its definition, causes, and symptoms. The language is clear and concise, making it accessible to readers without prior knowledge of the disease.
I found this overview informative but felt it was lacking specific examples or case studies demonstrating real-world impacts on healthcare systems worldwide especially concerning prevention efforts
I appreciate how this article highlights the complexity of leprosy as a multifaceted disease with varying clinical manifestations. However, I would like to see more emphasis on current research efforts aimed at improving diagnosis and treatment options.
This article does an excellent job explaining how Mycobacterium leprae infects cooler parts of the human body like skin and peripheral nerves but could benefit from additional graphics or diagrams illustrating this concept.
A well-written piece overall though consideration might need given discussing advancements made so far toward understanding exact mechanisms behind transmission alongside speculations mentioned within current understanding.