Introduction
Heart failure‚ a manifestation of cardiovascular disease‚ necessitates a comprehensive clinical evaluation. A thorough history and physical examination are crucial in diagnosing heart failure‚ guiding further investigation‚ and informing management strategies to mitigate symptoms and improve patient outcomes.
Symptoms of Heart Failure
Symptoms of heart failure are diverse and can vary significantly among individuals. They may be acute or chronic‚ mild or severe‚ and can affect various aspects of a patient’s life. Recognizing these symptoms is essential for early diagnosis and timely intervention.
Prompt identification of heart failure symptoms enables healthcare providers to initiate appropriate treatment‚ thereby improving quality of life‚ reducing morbidity‚ and decreasing mortality rates. Symptoms may be categorized into common and less common manifestations‚ each necessitating a distinct approach to clinical evaluation and management.
An understanding of the pathophysiological mechanisms underlying heart failure is crucial in interpreting patients’ symptoms and developing effective treatment plans. This knowledge facilitates healthcare providers to tailor their clinical assessment and therapeutic interventions to address the specific needs of each patient.
A thorough grasp of heart failure symptoms also facilitates communication between healthcare providers and patients‚ fostering a collaborative approach to care. By acknowledging the complexities of heart failure symptoms‚ clinicians can provide empathetic‚ patient-centered care‚ addressing the unique concerns and expectations of each individual.
Elucidating the symptoms of heart failure is an essential step in the diagnostic process‚ as it informs subsequent stages of clinical evaluation‚ including physical examination and diagnostic testing.
Common Symptoms
Common symptoms of heart failure include shortness of breath‚ fatigue‚ and swelling. Shortness of breath‚ or dyspnea‚ may occur at rest or with exertion and can be exacerbated by lying down. Fatigue is a pervasive symptom‚ affecting patients’ ability to perform daily activities and maintain their quality of life.
Swelling‚ or edema‚ typically affects the lower extremities‚ such as the feet‚ ankles‚ and legs. However‚ it can also occur in the abdomen‚ liver‚ and lungs. Patients may report weight gain due to fluid retention‚ which can be a subtle yet significant indicator of worsening heart failure.
Palpitations‚ or irregular heartbeats‚ are another common symptom of heart failure. Patients may experience skipped beats‚ extra beats‚ or a sensation of their heart racing or pounding. Chest pain‚ coughing‚ and wheezing can also occur‚ particularly if heart failure is complicated by coronary artery disease or pulmonary congestion.
These common symptoms can vary in severity and impact patients’ daily lives significantly. A thorough understanding of these symptoms enables healthcare providers to develop targeted treatment plans‚ addressing the unique needs of each patient and improving their overall quality of life.
Early recognition and management of common symptoms are crucial in mitigating the progression of heart failure and reducing the risk of complications and hospitalizations.
Less Common Symptoms
Less common symptoms of heart failure include nocturnal cough‚ insomnia‚ and decreased libido. Additionally‚ some patients may experience nausea‚ abdominal discomfort‚ or anorexia due to liver congestion or impaired gastrointestinal perfusion‚ further complicating the clinical presentation.
Medical History
A meticulous medical history is essential in the evaluation of patients with suspected heart failure. It provides valuable information regarding the underlying etiology‚ severity‚ and chronicity of the condition. A detailed history helps clinicians to identify potential risk factors‚ such as hypertension‚ diabetes mellitus‚ and coronary artery disease.
The medical history should also encompass a thorough review of the patient’s medication regimen‚ including current and past treatments. This information can help clinicians to assess potential pharmacological contributors to the development or exacerbation of heart failure.
Additionally‚ a comprehensive medical history should include inquiries about the patient’s lifestyle‚ including dietary habits‚ physical activity level‚ and tobacco use. This information can aid clinicians in identifying opportunities for lifestyle modification and optimization of treatment strategies.
Furthermore‚ a thorough medical history enables clinicians to assess the patient’s functional status and overall quality of life. This information can inform decisions regarding the need for further diagnostic testing‚ hospitalization‚ or referral to specialized care.
By obtaining a thorough medical history‚ clinicians can develop a more accurate understanding of the patient’s condition and create a personalized treatment plan that addresses their unique needs and circumstances.
Importance of Medical History
The medical history is a vital component of the diagnostic evaluation for heart failure‚ providing essential information that guides further investigation and informs management strategies. A thorough medical history enables clinicians to establish a temporal relationship between symptoms and potential precipitating factors.
An accurate medical history also facilitates the identification of comorbid conditions that may contribute to the development or exacerbation of heart failure‚ such as hypertension‚ diabetes mellitus‚ or chronic kidney disease. This information can aid clinicians in developing targeted interventions to address these underlying conditions.
Moreover‚ a comprehensive medical history helps clinicians to assess the patient’s risk profile and stratify them according to their likelihood of adverse outcomes. This information can inform decisions regarding the need for hospitalization‚ referral to specialized care‚ or initiation of specific treatments.
The importance of a thorough medical history cannot be overstated‚ as it sets the stage for a focused physical examination‚ judicious use of diagnostic testing‚ and development of a personalized treatment plan. By investing time and effort into obtaining a detailed medical history‚ clinicians can improve diagnostic accuracy‚ optimize treatment strategies‚ and ultimately enhance patient outcomes.
A well-conducted medical history is essential for delivering high-quality‚ patient-centered care in the context of heart failure.
Components of Medical History
A comprehensive medical history for heart failure includes chief complaint‚ history of present illness‚ past medical history‚ medications‚ allergies‚ social history‚ family history‚ and review of systems‚ providing a thorough understanding of the patient’s clinical presentation and relevant background information.
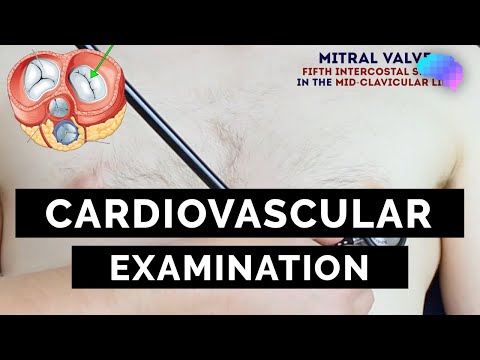
Physical Examination
A thorough physical examination is a crucial component of the diagnostic process for heart failure‚ providing valuable information regarding the severity and progression of the disease. A well-structured physical examination enables healthcare providers to assess the patient’s overall clinical status‚ identify potential signs of heart failure‚ and guide further investigation and management.
The physical examination for heart failure should be systematic and comprehensive‚ encompassing an assessment of vital signs‚ including pulse‚ blood pressure‚ respiratory rate‚ and oxygen saturation. A detailed evaluation of the cardiovascular system‚ including auscultation of the heart and lungs‚ palpation of the precordium‚ and assessment of peripheral pulses‚ is essential in identifying signs of cardiac dysfunction.
Additional components of the physical examination include inspection of the jugular venous pressure‚ palpation of the abdomen to detect signs of ascites or hepatomegaly‚ and assessment of the extremities for evidence of peripheral edema. A thorough physical examination provides a solid foundation for the diagnosis and management of heart failure‚ informing the selection of further diagnostic tests and guiding therapeutic interventions to optimize patient outcomes.
Auscultation
Auscultation is a critical component of the physical examination for heart failure‚ allowing healthcare providers to assess cardiac function and identify potential abnormalities. A thorough auscultation of the heart involves listening to the sounds produced by the heart valves and chambers during systole and diastole.
In patients with heart failure‚ auscultation may reveal a range of abnormal heart sounds‚ including murmurs‚ gallops‚ and clicks. Systolic murmurs‚ such as those caused by mitral regurgitation or aortic stenosis‚ may be indicative of left ventricular dysfunction or valvular disease. Diastolic murmurs‚ such as those associated with aortic regurgitation or mitral stenosis‚ may suggest conditions that can contribute to the development of heart failure.
The presence of a third heart sound (S3) or fourth heart sound (S4) may also be detected through auscultation. An S3 is often associated with left ventricular volume overload‚ while an S4 may indicate decreased ventricular compliance. Accurate identification and interpretation of these sounds are essential in diagnosing and managing heart failure‚ as they provide valuable insights into the underlying pathophysiology and guide further investigation and therapeutic interventions;
Jugular Venous Distension
Jugular venous distension (JVD) is a physical examination finding that can be indicative of heart failure‚ particularly right-sided heart failure. JVD is characterized by an elevated jugular venous pressure‚ which is typically assessed by observing the height of the jugular venous pulsations above the sternal angle.
To accurately assess JVD‚ patients are positioned at a 45-degree angle‚ and the jugular venous pulsations are observed. The vertical distance between the top of the jugular venous pulsation and the sternal angle is measured‚ with a distance greater than 2 cm indicating elevated jugular venous pressure.
The presence of JVD suggests increased pressure in the superior and inferior vena cava‚ which can be caused by right ventricular dysfunction or tricuspid regurgitation. In patients with heart failure‚ JVD is often accompanied by other signs of fluid overload‚ such as peripheral edema and pulmonary congestion. Accurate assessment and documentation of JVD are essential in diagnosing and managing heart failure‚ as this finding can inform decisions regarding fluid management and guide further investigation into the underlying causes of heart failure.
Peripheral Edema
Peripheral edema‚ a common manifestation of heart failure‚ is characterized by the accumulation of fluid in the interstitial spaces of the lower extremities. Pitting edema‚ typically observed in dependent areas‚ can be assessed by applying gentle pressure with the examiner’s finger.
Diagnostic Tests
Following a comprehensive history and physical examination‚ diagnostic tests are employed to confirm the diagnosis of heart failure‚ assess disease severity‚ and guide management strategies. A range of investigations may be utilized‚ including non-invasive and invasive modalities.
Non-invasive tests‚ such as radiographic studies and biomarker analysis‚ provide valuable information on cardiac structure and function. Electrocardiography (ECG) and Holter monitoring enable the evaluation of cardiac rhythm and arrhythmia detection.
Invasive testing‚ including cardiac catheterization and coronary angiography‚ may be necessary in select cases to assess coronary anatomy‚ measure hemodynamic parameters‚ and guide revascularization therapies.
Imaging modalities‚ such as cardiac magnetic resonance imaging (MRI) and computed tomography (CT)‚ offer detailed assessments of cardiac morphology and function. These investigations facilitate the diagnosis of underlying conditions contributing to heart failure‚ including coronary artery disease and cardiomyopathy.
Selective use of these diagnostic tests‚ in conjunction with clinical evaluation‚ enables healthcare providers to develop targeted treatment plans‚ monitor disease progression‚ and improve patient outcomes in heart failure.
Echocardiogram
An echocardiogram is a crucial diagnostic tool in the evaluation of heart failure‚ providing a non-invasive assessment of cardiac structure and function. This modality employs high-frequency sound waves to generate images of the heart‚ enabling the examination of ventricular dimensions‚ wall motion‚ and valvular function.
Two-dimensional (2D) and three-dimensional (3D) echocardiography facilitate the evaluation of left ventricular ejection fraction (LVEF)‚ a critical parameter in the diagnosis and management of heart failure. Doppler echocardiography allows for the assessment of blood flow velocities and pressure gradients across valves.
Echocardiography is also useful in identifying underlying conditions contributing to heart failure‚ including coronary artery disease‚ cardiomyopathy‚ and valvular heart disease. The technique is highly sensitive and specific for detecting abnormalities in cardiac function and structure.
The use of echocardiography in heart failure diagnosis and management is supported by clinical guidelines‚ which recommend its application in the initial evaluation and ongoing monitoring of patients with heart failure. By providing valuable information on cardiac function and structure‚ echocardiography informs treatment decisions and improves patient outcomes in heart failure.
Echocardiography is widely available‚ relatively inexpensive‚ and free of radiation exposure‚ making it an attractive diagnostic modality in the management of heart failure.
While this article provides an excellent foundation for understanding heart failure symptoms, I would have liked to see more exploration into emerging research areas or novel approaches being developed for symptom identification.
This article provides a comprehensive overview of the importance of recognizing symptoms in diagnosing heart failure. The emphasis on prompt identification and treatment is particularly noteworthy, as it highlights the significance of timely intervention in improving patient outcomes.
As a healthcare provider, I found this article informative and relevant to my practice. The discussion on pathophysiological mechanisms underlying heart failure is particularly useful, as it reinforces the importance of understanding these concepts when interpreting patient symptoms.
One area that could be improved upon is providing more concrete examples or case studies illustrating how symptom recognition has led to successful treatment outcomes in real-world scenarios.
The article effectively underscores the diversity of heart failure symptoms, which can often lead to delayed diagnosis if not properly recognized. I appreciate how the author stresses the need for a tailored approach to clinical evaluation and management.
I appreciate how this article emphasizes empathy and patient-centered care when addressing heart failure symptoms. This aspect is often overlooked but is crucial for building trust between healthcare providers and patients.