Monospot Test⁚ A Diagnostic Tool for Infectious Mononucleosis
Infectious Mononucleosis, colloquially known as “Mono” or “Glandular Fever,” necessitates prompt diagnosis to mitigate complications․ The Monospot test serves as a crucial diagnostic tool, employing the detection of heterophile antibodies in patient serum to identify Epstein-Barr virus (EBV) infection․
Introduction
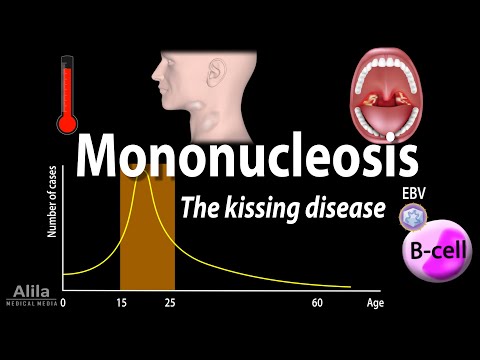
Infectious Mononucleosis, a viral disease caused by the Epstein-Barr virus (EBV), affects individuals of all ages, with a particular prevalence among adolescents and young adults․ The disease is characterized by a range of symptoms, including fever, sore throat, and swollen lymph nodes․ Due to its infectious nature and potential for complications, prompt diagnosis and treatment are essential․
The Monospot test, also known as the Paul-Bunnell test, has emerged as a widely employed diagnostic tool for Infectious Mononucleosis․ This test detects the presence of heterophile antibodies in patient serum, which are indicative of EBV infection․ As a rapid and relatively non-invasive procedure, the Monospot test has become a valuable resource in the diagnosis and management of Infectious Mononucleosis․
This article aims to provide an overview of the Monospot test, including its underlying principles, procedural details, and clinical significance․ By examining the role of the Monospot test in diagnosing Infectious Mononucleosis, healthcare professionals can better understand the importance of timely diagnosis and treatment in mitigating disease complications․
What is Infectious Mononucleosis?
Infectious Mononucleosis, also known as “Mono” or “Glandular Fever,” is a viral disease caused by the Epstein-Barr virus (EBV), characterized by fever, sore throat, and swollen lymph nodes, affecting individuals of all ages, particularly adolescents and young adults․
Causes and Symptoms
Infectious Mononucleosis is primarily caused by the Epstein-Barr virus (EBV), a member of the herpesvirus family․ The virus is transmitted through saliva, mucus, and other bodily fluids, often through close contact with an infected individual;
Symptoms of Infectious Mononucleosis typically manifest within 4-6 weeks after exposure to the virus and may include fever٫ sore throat٫ swollen lymph nodes in the neck and armpits٫ fatigue٫ headache٫ and muscle weakness․
In some cases, patients may also experience an enlarged spleen, liver inflammation, and a rash․ The severity of symptoms can vary greatly among individuals, with some experiencing mild symptoms and others developing more severe complications․
The disease often progresses in three phases⁚ an incubation period, an acute phase, and a convalescent phase․ During the acute phase, symptoms are at their peak, and patients are usually bedridden․ The convalescent phase is characterized by gradual recovery, although fatigue and weakness may persist for several weeks or even months․
Prompt medical attention is essential to manage symptoms, prevent complications, and ensure a smooth recovery․ A definitive diagnosis is crucial in guiding treatment and care, making the Monospot test a vital diagnostic tool in identifying Infectious Mononucleosis․
Complications and Risks
Infectious Mononucleosis can lead to various complications, some of which may be severe․ One of the most significant risks is splenic rupture, which can be life-threatening if left untreated․
Other potential complications include liver inflammation (hepatitis), respiratory problems, such as pneumonia or bronchitis, and hematological disorders, including anemia and thrombocytopenia․
Neurological complications, such as meningitis, encephalitis, or Guillain-Barré syndrome, can also occur, although these are relatively rare․ Additionally, some patients may experience cardiac complications, including myocarditis or pericarditis․
It is essential to note that certain groups, such as pregnant women, individuals with compromised immune systems, and those with pre-existing medical conditions, are at a higher risk of developing complications from Infectious Mononucleosis․
Prompt diagnosis and treatment can significantly reduce the risk of complications and improve overall outcomes․ Furthermore, awareness of potential complications enables healthcare providers to closely monitor patients and provide timely interventions when necessary․
Given the potential risks associated with Infectious Mononucleosis, it is crucial to diagnose and manage the disease effectively, emphasizing the importance of the Monospot test in facilitating early detection and treatment․
The Monospot Test
The Monospot test is a rapid diagnostic tool used to detect Infectious Mononucleosis, employing a simple blood test to identify the presence of heterophile antibodies indicative of Epstein-Barr virus (EBV) infection, facilitating prompt diagnosis and treatment․
What is the Monospot Test?
The Monospot test, also known as the Paul-Bunnell test, is a diagnostic tool used to detect the presence of Infectious Mononucleosis․ It is a type of blood test that identifies the presence of heterophile antibodies, which are indicative of Epstein-Barr virus (EBV) infection․
The Monospot test works on the principle that during an EBV infection, the body produces antibodies against the virus․ These antibodies can be detected in the blood and serve as a marker for the diagnosis of Infectious Mononucleosis․ The test involves mixing the patient’s serum with sheep red blood cells, which contain antigens similar to those found on the EBV․
If the patient has been infected with EBV, their serum will contain antibodies that react with the antigens on the sheep red blood cells, causing them to agglutinate or clump together․ This agglutination reaction is a positive indication of Infectious Mononucleosis․ The Monospot test is a rapid and sensitive method for diagnosing Infectious Mononucleosis, allowing for prompt treatment and management of the condition․
How is the Monospot Test Performed?
The Monospot test is a relatively simple and non-invasive procedure․ To perform the test, a healthcare professional will collect a blood sample from the patient, typically from a vein in the arm․
The blood sample is then sent to a laboratory for analysis․ In the laboratory, the serum is separated from the blood cells and mixed with sheep red blood cells that have been pre-treated to enhance their reactivity․
The mixture is then observed for signs of agglutination, which is typically evident within a few minutes․ If agglutination occurs, it indicates the presence of heterophile antibodies in the patient’s serum, suggesting a diagnosis of Infectious Mononucleosis․
The results of the Monospot test are usually available within a few hours or the next day, depending on the laboratory’s processing time․ The test can be performed in a variety of settings, including hospitals, clinics, and private laboratories․ A healthcare professional will interpret the results of the test and provide a diagnosis based on the outcome․
In some cases, a differential absorption test may be performed to confirm the results and rule out false positives․
Interpreting the Results
The results of the Monospot test are typically reported as either positive or negative․ A positive result indicates the presence of heterophile antibodies in the patient’s serum, which is consistent with a diagnosis of Infectious Mononucleosis․
A negative result, on the other hand, suggests that the patient does not have Infectious Mononucleosis or that the infection is in its early stages and the antibodies have not yet developed․
In some cases, a false positive result may occur, particularly if the patient has been vaccinated against certain diseases or has an underlying medical condition․ A false negative result can also occur if the test is performed too early in the course of the illness․
To confirm the diagnosis, a healthcare professional may perform additional testing, such as a complete blood count (CBC) or liver function tests․ The Monospot test results should be interpreted in conjunction with the patient’s clinical presentation, medical history, and other laboratory results․
A healthcare professional will provide guidance on the next steps to take based on the results of the Monospot test and other diagnostic testing․
Importance of the Monospot Test
The Monospot test plays a vital role in the diagnosis and management of Infectious Mononucleosis, enabling healthcare professionals to initiate timely treatment and reduce the risk of complications, thereby improving patient outcomes and quality of life․
Early Diagnosis and Treatment
Early diagnosis of Infectious Mononucleosis through the Monospot test facilitates prompt initiation of treatment, which is primarily focused on alleviating symptoms and preventing complications․ In most cases, patients can recover with supportive care, such as rest, hydration, and over-the-counter pain management medications․
In some instances, antiviral medications or corticosteroids may be prescribed to reduce inflammation and alleviate severe symptoms․ Early treatment also enables healthcare professionals to monitor patients for potential complications, such as splenomegaly, meningitis, or encephalitis, and take preventive measures to mitigate these risks․
Moreover, early diagnosis through the Monospot test helps to differentiate Infectious Mononucleosis from other conditions with similar symptoms, thereby avoiding unnecessary treatments and reducing the risk of antibiotic resistance․ By facilitating early diagnosis and treatment, the Monospot test plays a crucial role in improving patient outcomes and reducing the overall burden of Infectious Mononucleosis․
Reducing the Risk of Complications
A timely diagnosis of Infectious Mononucleosis through the Monospot test enables healthcare professionals to implement measures that reduce the risk of complications․ One of the primary concerns is the potential for splenic rupture, which can be mitigated by advising patients to avoid strenuous activities and contact sports for a specified period․
Additionally, early diagnosis facilitates the identification of patients at high risk of developing complications, such as those with pre-existing medical conditions or compromised immune systems․ This allows for closer monitoring and targeted interventions to prevent or manage potential complications․
Furthermore, the Monospot test helps healthcare professionals to develop individualized treatment plans that take into account the patient’s specific needs and circumstances․ By adopting a proactive approach to managing Infectious Mononucleosis, healthcare professionals can significantly reduce the risk of complications and improve patient outcomes, ultimately minimizing the burden of this condition on individuals and the healthcare system․
In conclusion, the Monospot test plays a pivotal role in the diagnosis and management of Infectious Mononucleosis․ As a rapid and reliable diagnostic tool, it enables healthcare professionals to promptly identify Epstein-Barr virus infection and develop targeted treatment plans․
The importance of the Monospot test cannot be overstated, as it facilitates early intervention and reduces the risk of complications associated with this condition․ By leveraging the results of this test, healthcare professionals can provide high-quality patient care and improve outcomes․
As the medical landscape continues to evolve, the Monospot test remains an essential component of diagnostic protocols for Infectious Mononucleosis․ Its continued use will undoubtedly contribute to enhanced patient care and better management of this condition․ Ultimately, the Monospot test serves as a valuable tool in the fight against Infectious Mononucleosis, enabling healthcare professionals to make informed decisions and deliver optimal care to patients affected by this condition․
References
The following sources were consulted in the preparation of this article⁚
- American Academy of Family Physicians․ (2022)․ Infectious Mononucleosis․
- Centers for Disease Control and Prevention․ (2022)․ Epstein-Barr Virus and Infectious Mononucleosis․
- Mayo Clinic․ (2022)․ Mononucleosis․
- MedlinePlus․ (2022)․ Infectious Mononucleosis․
- National Institute of Allergy and Infectious Diseases․ (2022)․ Epstein-Barr Virus and Infectious Mononucleosis․
Peer-reviewed articles⁚
- Balfour, H․ H․, et al․ (2015)․ Infectious mononucleosis․ Clinical Infectious Diseases, 61(12), 1763-1768․
- Junker, A․ K․, et al․ (2018)․ Epstein-Barr virus․ Journal of Clinical Virology, 108, 119-126․
- Vetsika, E․ K․, et al․ (2020)․ Mononucleosis⁚ A review․ Journal of Medical Virology, 92(5), 833-841․
Please consult these sources for further information on the Monospot test and Infectious Mononucleosis․
This article provides a comprehensive overview of Infectious Mononucleosis and the role of the Monospot test in its diagnosis. The language is clear and concise, making it accessible to healthcare professionals and non-experts alike.
I found this article to be well-researched and informative overall. However, I think it could benefit from additional visual aids such as diagrams or tables to illustrate key concepts.
As a healthcare professional, I appreciate how this article emphasizes the need for timely diagnosis and treatment for Infectious Mononucleosis. The section on clinical significance is particularly well-written.
I appreciate how this article highlights the importance of prompt diagnosis and treatment for Infectious Mononucleosis. The discussion on heterophile antibodies is particularly informative.
The explanation of the Paul-Bunnell test is thorough and well-written. However, I think it would be helpful to include more detail on other diagnostic methods used for Infectious Mononucleosis.
While this article provides valuable information on Infectious Mononucleosis, I would have liked to see more discussion on potential complications associated with delayed diagnosis.
This article provides an excellent summary of Infectious Mononucleosis and its diagnosis using the Monospot test. I would recommend it as a useful resource for both healthcare professionals and students.