Placenta Accreta⁚ A Serious Pregnancy Complication
Placenta accreta is a rare yet severe pregnancy complication characterized by abnormal placental invasion into the uterine wall, posing significant risks to both maternal health and fetal development, necessitating prompt medical attention.
Introduction
Placenta accreta is a complex and potentially life-threatening condition that affects pregnant women worldwide. Despite its rarity, the incidence of placenta accreta has increased significantly over the past few decades, largely due to the rising rates of cesarean deliveries and other uterine surgeries. This condition poses a considerable challenge to obstetricians and pregnant women alike, as it can lead to severe complications during pregnancy, childbirth, and postpartum.
A thorough understanding of placenta accreta is essential for providing optimal prenatal care and minimizing the risks associated with this condition. This article aims to provide a comprehensive overview of placenta accreta, including its causes, symptoms, diagnosis, and treatment options. By exploring the complexities of this condition, healthcare providers can develop more effective strategies for managing placenta accreta and improving outcomes for affected women and their families.
Through a multidisciplinary approach, we can work towards reducing the morbidity and mortality rates associated with placenta accreta and promoting better reproductive health for women worldwide.
Causes and Risk Factors
Multiparity, prior cesarean delivery, and history of uterine surgery are significant risk factors for placenta accreta, as they can lead to abnormal placental invasion and uterus attachment complications during pregnancy.
Placental Invasion and Uterus Attachment
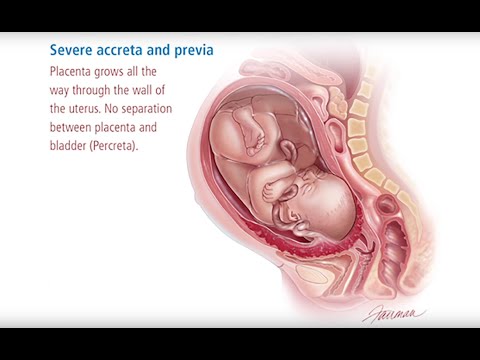
Placenta accreta is characterized by the abnormal invasion of placental tissue into the uterine wall, which can lead to a spectrum of complications. The normal placental invasion process involves the invasion of trophoblast cells into the decidua basalis, allowing for the establishment of a healthy placenta. However, in placenta accreta, this process is disrupted, resulting in the invasion of placental tissue into the myometrium.
This abnormal invasion can lead to varying degrees of uterus attachment, ranging from placenta accreta, where the placenta invades the myometrium, to placenta increta, where the placenta invades the entire myometrium, and placenta percreta, where the placenta invades through the uterine wall and into surrounding organs. Understanding the mechanisms of placental invasion and uterus attachment is crucial for the diagnosis and management of placenta accreta.
The degree of placental invasion and uterus attachment plays a significant role in determining the severity of symptoms and complications associated with placenta accreta. Accurate diagnosis and assessment of the extent of placental invasion are essential for developing effective treatment strategies and minimizing maternal and fetal risks.
Symptoms and Complications
Placenta accreta often presents with vaginal bleeding in the third trimester, which can be life-threatening for both mother and fetus, necessitating prompt medical attention to prevent severe pregnancy complications and ensure optimal outcomes.
Vaginal Bleeding and Pregnancy Complications
Vaginal bleeding is a hallmark symptom of placenta accreta, often occurring in the absence of pain. The bleeding can be heavy and life-threatening, posing significant risks to both maternal and fetal health. In some cases, the bleeding may be accompanied by other symptoms such as abdominal pain, uterine tenderness, and premature labor.
The vaginal bleeding associated with placenta accreta can lead to severe pregnancy complications, including shock, disseminated intravascular coagulation, and acute kidney injury. Furthermore, the bleeding can compromise fetal well-being, resulting in growth restriction, preterm birth, and even fetal demise.
It is essential to recognize the severity of vaginal bleeding in placenta accreta and provide prompt medical attention to prevent these complications; A multidisciplinary approach, involving obstetricians, anesthesiologists, and other specialists, is crucial in managing these high-risk pregnancies and ensuring optimal outcomes for both mother and fetus.
Diagnosis and Treatment
Diagnosis and treatment of placenta accreta involve a multidisciplinary approach, incorporating imaging studies, such as ultrasound and MRI, and surgical interventions, including cesarean delivery, to manage this high-risk condition effectively.
Prenatal Diagnosis and Obstetric Care
A prenatal diagnosis of placenta accreta is crucial for optimal obstetric care. Imaging studies, such as transvaginal ultrasound and MRI, play a vital role in identifying abnormal placental invasion. In cases where placenta accreta is suspected, a multidisciplinary team should be assembled to provide comprehensive care.
Women with a history of uterine surgery or placenta previa are at increased risk of developing placenta accreta. Therefore, they should receive close surveillance throughout their pregnancy. A thorough evaluation of the placenta and uterus should be conducted to assess the extent of placental invasion and guide treatment decisions.
Obstetric care providers should be aware of the potential complications associated with placenta accreta and have a clear plan in place for managing emergencies. This includes having a skilled surgical team on standby and ensuring that the patient has access to blood products and other necessary resources.
Maternal and Fetal Risks
Placenta accreta poses significant risks to both mother and fetus, including severe vaginal bleeding, childbirth risks, and life-threatening complications necessitating immediate medical intervention and potential cesarean delivery.
Childbirth Risks and Maternal Health
Placenta accreta significantly increases the risk of severe complications during childbirth, posing a substantial threat to maternal health. The abnormal placental attachment can lead to catastrophic bleeding, necessitating massive transfusions and potentially life-saving interventions. Furthermore, the condition heightens the risk of placenta previa, where the placenta partially or completely covers the cervix, further complicating delivery.
In extreme cases, placenta accreta may require a hysterectomy to control hemorrhaging, resulting in permanent infertility. Additionally, the condition can lead to cardiac arrest, acute respiratory distress syndrome, and other life-threatening complications. It is crucial that women with suspected placenta accreta receive close monitoring and care from a multidisciplinary team of specialists to mitigate these risks and ensure the best possible outcomes for both mother and baby.
In some cases, women may be placed on bed rest or hospitalized for extended periods to minimize the risk of preterm labor and associated complications. Despite these measures, placenta accreta remains a leading cause of maternal morbidity and mortality worldwide.
Prevention and Management
Although placenta accreta cannot be entirely prevented, meticulous prenatal diagnosis and targeted interventions can significantly mitigate risks, ensuring optimal outcomes through comprehensive obstetric care and strategic delivery planning.
Early Detection and Intervention
Early detection of placenta accreta is crucial for effective management. A multidisciplinary approach, involving obstetricians, radiologists, and other specialists, is essential for accurate diagnosis and timely intervention.
Ultrasound imaging and MRI scans can help identify placental invasion and uterine attachment abnormalities, enabling healthcare providers to develop targeted treatment plans. In some cases, amniocentesis or chorionic villus sampling may be necessary to confirm the diagnosis.
Prompt intervention can significantly improve maternal and fetal outcomes. Women with suspected placenta accreta should be closely monitored and delivered at a tertiary care center with a multidisciplinary team experienced in managing this condition. In some cases, prophylactic hysterectomy or uterine artery embolization may be necessary to prevent severe bleeding complications.
A well-coordinated management plan, including early detection, close monitoring, and strategic delivery planning, is essential for optimizing outcomes in women with placenta accreta.
The discussion on risk factors for placenta accreta is well-done; however, I would have liked to see more information on genetic predispositions to this condition.
The section on placental invasion and uterus attachment could benefit from additional illustrations or diagrams to help readers visualize these complex processes.
This article provides a comprehensive overview of placenta accreta, highlighting its causes, symptoms, diagnosis, and treatment options. As an obstetrician, I appreciate the emphasis on multidisciplinary approaches to managing this condition.
As someone who has experienced placenta accreta firsthand, I appreciate the attention given to this often-overlooked condition. More awareness needs to be raised about its potential risks.