Pneumocystis Pneumonia⁚ A Life-Threatening Opportunistic Infection
Pneumocystis pneumonia (PCP) is a severe and potentially life-threatening opportunistic infection that affects individuals with weakened immune systems, particularly those with HIV/AIDS, causing significant morbidity and mortality worldwide.
Introduction to Pneumocystis carinii
Pneumocystis carinii, now reclassified as Pneumocystis jirovecii, is a unique and highly specialized fungus that is the causative agent of Pneumocystis pneumonia (PCP). Initially identified as a protozoan, this microorganism was later classified as a fungus based on molecular and genetic analysis. Pneumocystis carinii was first described in the 1950s as a rare cause of pneumonia in immunocompromised individuals. However, with the advent of the HIV/AIDS epidemic, PCP emerged as a major opportunistic infection, highlighting the significance of this pathogen in clinical medicine. Despite advances in antiretroviral therapy and prophylactic measures, PCP remains a significant challenge in the management of immunocompromised patients. Understanding the biology and epidemiology of Pneumocystis carinii is crucial for the development of effective diagnostic and therapeutic strategies against this pathogen.
Clinical Presentation of PCP
The clinical presentation of Pneumocystis pneumonia (PCP) is characterized by nonspecific respiratory symptoms, including coughing, fever, and shortness of breath, which can progress to severe respiratory distress in immunocompromised individuals if left untreated.
Pneumonia Symptoms
The symptoms of Pneumocystis pneumonia (PCP) can vary in severity and may develop gradually over several weeks or rapidly over a few days. Common pneumonia symptoms include coughing, which may be dry or produce thin, white or pink-tinged mucus, fever, chills, shortness of breath or difficulty breathing, chest tightness or discomfort, and fatigue. In severe cases, PCP can cause respiratory failure, which may lead to hypoxia, or low levels of oxygen in the blood, and require mechanical ventilation to support breathing.
In addition to these respiratory symptoms, some individuals with PCP may also experience systemic symptoms, such as weight loss, night sweats, and loss of appetite. It is essential to seek medical attention promptly if symptoms persist or worsen over time, as early diagnosis and treatment are critical in preventing serious complications and improving outcomes.
The Biology of Pneumocystis
Pneumocystis is a genus of fungi that infects the lungs of mammals, with P. jirovecii being the species responsible for human infections, exhibiting a complex life cycle and unique characteristics.
Cystic and Trophic Forms
The life cycle of Pneumocystis involves two primary forms⁚ the cystic form and the trophic form. The cystic form, also known as the ascus, is a thick-walled, spherical structure that contains eight intracystic bodies or spores.
The cystic form is responsible for transmission and infection, as it is highly resistant to environmental stressors and can survive outside of a host for extended periods. In contrast, the trophic form is a thin-walled, ameboid structure that is responsible for colonization and replication within the host lung tissue.
The trophic form is the predominant stage found in infected individuals and is characterized by its ability to adhere to alveolar epithelial cells, where it undergoes repeated cycles of binary fission to produce large numbers of organisms, ultimately leading to the development of pneumonia.
Understanding the different forms of Pneumocystis is essential for the development of effective diagnostic and therapeutic strategies against this opportunistic pathogen.
PCP in Immunocompromised Patients
Pneumocystis pneumonia predominantly affects immunocompromised patients, particularly those with compromised cell-mediated immunity, increasing their susceptibility to this opportunistic infection and its life-threatening consequences if left untreated.
HIV/AIDS and PCP Risk
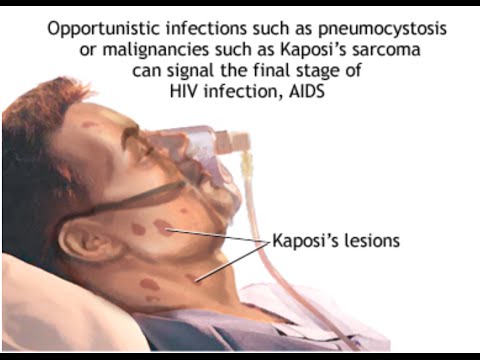
Individuals with HIV/AIDS are at a significantly increased risk of developing Pneumocystis pneumonia, particularly when their CD4 cell count falls below 200 cells/μL. This correlation between HIV/AIDS and PCP risk is attributed to the compromised immune system’s inability to effectively combat opportunistic infections.
Pneumocystis pneumonia is often considered an AIDS-defining illness, highlighting the advanced stage of immunocompromise in these patients. The impaired cell-mediated immunity in HIV/AIDS patients renders them more susceptible to PCP, emphasizing the importance of prophylactic measures and early diagnosis in this high-risk population.
The interplay between HIV/AIDS and Pneumocystis pneumonia underscores the need for comprehensive management strategies, addressing both the underlying immunodeficiency and the opportunistic infection itself. By recognizing the heightened PCP risk in HIV/AIDS patients, healthcare providers can implement targeted interventions to mitigate this life-threatening complication.
Diagnosis and Treatment of PCP
Timely diagnosis and effective treatment of Pneumocystis pneumonia are crucial to reducing morbidity and mortality, necessitating a multidisciplinary approach that incorporates clinical evaluation, laboratory testing, and targeted therapeutic interventions.
Diagnostic Challenges
Diagnosing Pneumocystis pneumonia poses significant challenges due to its nonspecific clinical presentation, which can mimic other respiratory illnesses. The lack of a gold standard diagnostic test further complicates the process. Clinicians must rely on a combination of clinical evaluation, laboratory tests, and imaging studies to make an accurate diagnosis.
Bronchoalveolar lavage (BAL) and induced sputum analysis are commonly employed methods for detecting Pneumocystis organisms in respiratory specimens. However, these techniques require specialized equipment and expertise, limiting their availability in resource-constrained settings. Furthermore, the sensitivity and specificity of these tests can vary depending on the quality of the specimen and the expertise of the technician performing the analysis.
A definitive diagnosis of PCP often requires a comprehensive evaluation of the patient’s clinical history, physical examination findings, laboratory results, and radiographic imaging studies, highlighting the need for a multidisciplinary approach to diagnosis.
Treatment Strategies
The treatment of choice for Pneumocystis pneumonia (PCP) is trimethoprim-sulfamethoxazole (TMP-SMX), which targets the folic acid synthesis pathway essential for the organism’s growth and replication. This antimicrobial combination is effective in treating PCP, but its use can be limited by adverse reactions, particularly in HIV-infected patients.
Alternative treatment options, such as pentamidine and atovaquone, are available for patients intolerant to TMP-SMX or with treatment failure. However, these alternatives may have reduced efficacy or increased toxicity. In severe cases of PCP, corticosteroids may be added to the treatment regimen to reduce inflammation and prevent respiratory failure.
It is crucial to initiate treatment promptly, as delays can significantly worsen outcomes. A multidisciplinary approach, involving infectious disease specialists, pulmonologists, and other healthcare professionals, is often necessary to optimize treatment strategies and manage potential complications in patients with PCP.
Prevention and Prophylaxis
Effective prevention and prophylaxis strategies are crucial in reducing the incidence of Pneumocystis pneumonia (PCP) in high-risk populations, primarily through the use of chemoprophylaxis and judicious management of underlying immunosuppressive conditions.
Preventing PCP in High-Risk Patients
Preventing Pneumocystis carinii pneumonia (PCP) in high-risk patients requires a multifaceted approach. Patients with HIV/AIDS, cancer, or those undergoing immunosuppressive therapy should be considered for chemoprophylaxis. Trimethoprim-sulfamethoxazole (TMP-SMX) is the preferred agent, but alternative regimens such as dapsone or pentamidine may be used in cases of intolerance.
In addition to chemoprophylaxis, other preventive measures include avoiding exposure to potential sources of Pneumocystis, practicing good hygiene, and ensuring adequate nutrition and overall health; Identifying and managing underlying conditions that increase the risk of PCP is also crucial. Healthcare providers should remain vigilant and monitor high-risk patients closely for signs and symptoms of PCP, allowing for prompt initiation of treatment if the disease develops.
By adopting these preventive strategies, healthcare providers can significantly reduce the incidence of PCP in high-risk patients and improve their overall quality of life.
Future Directions in PCP Management
Research into Pneumocystis carinii pneumonia (PCP) continues to evolve, with several promising areas of investigation. Novel diagnostic techniques, such as molecular assays and imaging studies, are being developed to improve the accuracy and speed of diagnosis.
New therapeutic agents, including antifungal compounds and immunomodulators, are being explored as potential treatments for PCP. Additionally, studies on the genetic and environmental factors that contribute to the development of PCP may lead to the identification of novel targets for prevention and treatment.
Furthermore, efforts to develop an effective vaccine against Pneumocystis are underway. The development of such a vaccine would have a significant impact on public health, particularly in regions with high HIV/AIDS prevalence. As our understanding of PCP pathogenesis and host-pathogen interactions expands, we can expect to see the development of more effective management strategies and improved outcomes for patients with this life-threatening disease.
I found this article informative but would suggest incorporating more data on global incidence rates to provide context for readers unfamiliar with PCP
I commend the authors for their thorough discussion on the biology and epidemiology of Pneumocystis carinii. This knowledge is essential for developing effective diagnostic and therapeutic strategies against PCP.
This article serves as an excellent resource for those interested in learning about opportunistic infections affecting vulnerable populations.
This article effectively highlights the challenges posed by PCP despite advances in antiretroviral therapy and prophylactic measures.
I appreciate how this article underscores the need for continued awareness about opportunistic infections like PCP among healthcare professionals.
Overall, I am impressed by this well-researched article
While I agree with most points made in this article, I believe it would benefit from additional information on current research into novel treatments for PCP.
This article provides an excellent overview of Pneumocystis pneumonia (PCP), highlighting its significance as an opportunistic infection affecting immunocompromised individuals worldwide.
As someone working with HIV/AIDS patients, I appreciate how this article emphasizes the importance of understanding PCP