Introduction to Prostate Cancer Diagnosis
Prostate cancer diagnosis involves a comprehensive approach, incorporating clinical evaluation, laboratory tests, and imaging studies to accurately identify and stage the disease, enabling informed treatment decisions and optimal patient outcomes.
Initial Screening Methods
Early detection of prostate cancer relies on effective screening methods to identify individuals at high risk of developing the disease. A combination of clinical examination and laboratory tests enables healthcare professionals to assess prostate health and detect potential abnormalities.
The primary objective of initial screening is to identify asymptomatic men with prostate cancer, as early intervention significantly improves treatment outcomes. A thorough medical history, including familial predisposition and previous urological conditions, informs the selection of screening tests.
Initial screening methods are non-invasive and relatively painless, encouraging men to undergo regular assessment. Healthcare providers utilize a systematic approach, incorporating clinical evaluation and laboratory analysis to determine whether further diagnostic testing is warranted.
A well-structured screening program facilitates timely detection, reducing the risk of advanced disease and associated complications. By identifying men at increased risk, clinicians can provide personalized guidance on risk reduction strategies and recommend follow-up evaluations as necessary.
An overview of the primary initial screening methods employed in prostate cancer diagnosis will be discussed in the following sections, highlighting their roles in the early detection of the disease.
2.1 Digital Rectal Exam (DRE)
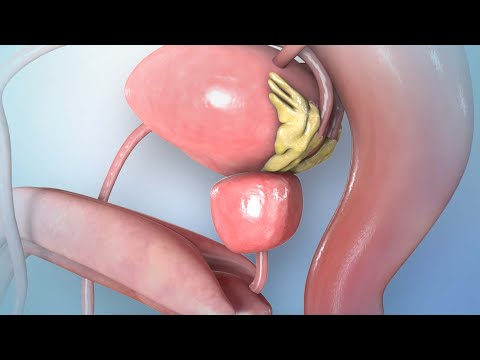
The digital rectal exam (DRE) is a fundamental component of prostate cancer screening, allowing healthcare professionals to assess the prostate gland for abnormalities. During the examination, a clinician inserts a gloved, lubricated finger into the rectum to palpate the prostate.
The DRE enables assessment of prostate size, consistency, and symmetry, as well as detection of any nodules or irregularities. A normal prostate feels smooth and even, while an abnormal prostate may exhibit areas of hardness or lumps.
Although the DRE is not definitive in diagnosing prostate cancer, it can identify suspicious lesions or abnormalities that warrant further investigation. A DRE is often performed in conjunction with other screening tests to provide a comprehensive evaluation of prostate health.
It is essential for clinicians to perform the DRE in a systematic and thorough manner to minimize the risk of missing significant abnormalities. The examination should be conducted with sensitivity and respect for the patient’s comfort and dignity.
A properly performed DRE can contribute significantly to the early detection of prostate cancer, particularly when combined with other screening modalities. Effective communication between the clinician and patient is crucial to ensure a successful examination and facilitate informed decision-making.
2.2 Prostate Specific Antigen (PSA) Test
The PSA test measures the level of prostate-specific antigen in the blood, a protein produced by the prostate gland. Elevated PSA levels may indicate prostate cancer, but can also result from benign conditions, requiring careful interpretation and further evaluation.
Imaging Tests for Prostate Cancer
Imaging tests play a crucial role in the diagnosis and staging of prostate cancer, providing valuable information on the extent and spread of the disease. These tests help identify potential areas of cancer, guide biopsies, and inform treatment decisions.
A range of imaging modalities is available, each with its strengths and limitations. The choice of imaging test depends on various factors, including the patient’s overall health, medical history, and clinical presentation. Imaging tests can help assess the local extent of the tumor, detect lymph node involvement, and identify distant metastases.
Advances in imaging technology have significantly improved the accuracy and sensitivity of these tests, enabling healthcare providers to diagnose and manage prostate cancer more effectively. A comprehensive understanding of the different imaging tests and their applications is essential for optimal patient care and outcomes.
In the following sections, we will discuss the various imaging tests used in prostate cancer diagnosis, including transrectal ultrasound, MRI scan, CT scan, and bone scan. Each of these tests provides unique information and plays a vital role in the diagnostic process.
3.1 Transrectal Ultrasound (TRUS)
Transrectal ultrasound (TRUS) is a widely used imaging modality in the diagnosis and management of prostate cancer. This test involves the insertion of an ultrasound probe into the rectum to visualize the prostate gland.
TRUS provides high-resolution images of the prostate, allowing healthcare providers to assess the size, shape, and structure of the gland. This information can help identify potential areas of cancer, guide biopsies, and monitor treatment response.
During a TRUS procedure, the ultrasound probe emits high-frequency sound waves that bounce off internal structures, producing detailed images of the prostate. The test is typically performed in conjunction with a biopsy, where tissue samples are collected for histopathological examination.
TRUS is a relatively quick and well-tolerated procedure, usually taking around 15-30 minutes to complete. While some discomfort may be experienced, it is generally minimal and temporary. The results of the TRUS examination are interpreted by a qualified healthcare professional, who will discuss the findings and any necessary next steps with the patient.
The use of TRUS has become a standard practice in urology, facilitating accurate diagnoses and effective management of prostate cancer.
3.2 MRI Scan
Magnetic Resonance Imaging (MRI) is a non-invasive diagnostic modality that provides detailed images of the prostate gland and surrounding tissues. This test is particularly useful in the evaluation of prostate cancer, as it can help identify tumors and assess their aggressiveness.
During an MRI scan, a strong magnetic field and radio waves are used to generate detailed images of the prostate. The test is typically performed with a specialized coil placed around the pelvic area to enhance image quality.
MRI scans can provide valuable information on tumor size, location, and extent of disease. This information can be used to guide biopsies, plan treatment, and monitor response to therapy.
One of the benefits of MRI is its ability to visualize the prostate in multiple planes, allowing for a more accurate assessment of tumor dimensions and relationships to adjacent structures.
The results of an MRI scan are interpreted by a qualified radiologist, who will report the findings to the patient’s healthcare provider. The use of MRI in prostate cancer diagnosis has become increasingly important, offering a powerful tool for improving diagnostic accuracy and guiding effective treatment strategies.
MRI scans are usually performed on an outpatient basis, and the procedure typically takes about 30-60 minutes to complete.
3.3 CT Scan
Computed Tomography (CT) scans utilize X-rays and computer technology to produce detailed cross-sectional images of the body, including the prostate gland and surrounding tissues.
In the context of prostate cancer diagnosis, CT scans are primarily used to assess for potential metastasis to lymph nodes, bones, or other organs. This information is crucial in determining the stage of disease and guiding treatment decisions.
During a CT scan, the patient lies on a table that slides into a large, doughnut-shaped machine. The test typically takes 10-30 minutes to complete, depending on the specific protocol and number of images required.
CT scans provide valuable information on the size and location of lymph nodes, as well as the presence of any metastatic disease in distant organs. However, they are not as sensitive as MRI scans in detecting tumors within the prostate gland itself.
The results of a CT scan are interpreted by a qualified radiologist, who will report the findings to the patient’s healthcare provider. In some cases, additional imaging tests or biopsies may be recommended based on the CT scan results.
It is essential to note that CT scans involve exposure to ionizing radiation, and patients should discuss any concerns or questions with their healthcare provider prior to undergoing the test.
3.4 Bone Scan
A bone scan is a nuclear medicine test that detects areas of abnormal bone metabolism, which can indicate prostate cancer metastasis. Small amounts of radioactive material are injected into the patient, and images are taken to visualize potential bone involvement.
Prostate Biopsy and Staging
Prostate biopsy and staging are crucial steps in the diagnostic process, providing essential information for guiding treatment decisions and predicting patient outcomes. A comprehensive evaluation of the prostate gland is necessary to determine the presence, extent, and aggressiveness of cancer.
The primary goal of prostate biopsy and staging is to assess the histopathological characteristics of the tumor, including its grade, volume, and anatomical location. This information enables clinicians to categorize patients into distinct risk groups, facilitating personalized management strategies.
An accurate assessment of prostate cancer stage is vital for selecting the most effective treatment approach, as it directly impacts the likelihood of achieving optimal therapeutic outcomes. Furthermore, precise staging helps identify patients who may benefit from active surveillance, thereby avoiding unnecessary interventions and minimizing potential treatment-related complications.
A well-coordinated multidisciplinary effort between urologists, radiologists, and pathologists is essential for ensuring accurate prostate biopsy and staging results. By combining clinical expertise with advanced diagnostic techniques, healthcare providers can provide high-quality care and improve patient prognosis.
4.1 Prostate Biopsy Procedure
The prostate biopsy procedure involves the systematic collection of tissue samples from the prostate gland, typically performed under local anesthesia to minimize patient discomfort. There are several approaches to prostate biopsy, including transrectal, transperineal, and transurethral methods.
The transrectal ultrasound-guided biopsy is the most commonly employed technique, which utilizes real-time ultrasound imaging to visualize the prostate gland and guide the biopsy needle. A predetermined number of tissue cores are obtained from various regions of the prostate, ensuring representative sampling of the gland.
To optimize biopsy accuracy, some clinicians employ advanced imaging modalities, such as magnetic resonance imaging (MRI) or fusion imaging, to target specific areas of suspicion within the prostate. These techniques may improve the detection rate of clinically significant cancers while reducing the risk of sampling errors.
Following the biopsy procedure, tissue samples are submitted for histopathological examination by a qualified pathologist, who evaluates the specimens for evidence of malignant transformation, tumor grade, and other relevant features. The resulting biopsy report provides essential information for guiding subsequent management decisions and determining the need for further diagnostic evaluation.
4.2 Prostate Cancer Staging
Prostate cancer staging is a critical component of the diagnostic process, as it provides essential information regarding the extent and spread of the disease. The most widely employed staging system for prostate cancer is the tumor, node, metastasis (TNM) classification.
The TNM system assesses three key aspects of the disease⁚ the primary tumor (T), regional lymph node involvement (N), and distant metastasis (M). Each category is further subdivided into specific subcategories, allowing for a more precise characterization of the disease.
The clinical stage of prostate cancer is determined by a combination of physical examination findings, imaging studies, and biopsy results. Additional diagnostic tests, such as computed tomography (CT) scans and bone scans, may be employed to evaluate for distant metastasis or lymph node involvement.
The American Joint Committee on Cancer (AJCC) has established guidelines for prostate cancer staging, which provide a standardized framework for clinicians to classify and manage patients with prostate cancer. Accurate staging is crucial in determining the most effective treatment strategy and predicting patient outcomes, emphasizing the importance of thorough and meticulous diagnostic evaluation.
4.3 Gleason Score
The Gleason score is a histopathological grading system, evaluating tumor aggressiveness based on glandular patterns and cellular differentiation, with scores ranging from 2 to 10, providing crucial prognostic information for guiding treatment decisions and predicting patient outcomes.
Conclusion
Prostate cancer diagnosis is a complex and multifaceted process, requiring a comprehensive approach that incorporates clinical evaluation, laboratory tests, and imaging studies. Accurate diagnosis and staging are crucial for guiding treatment decisions and predicting patient outcomes.
A thorough understanding of the diagnostic procedures and tools available is essential for healthcare professionals to provide optimal care for patients with prostate cancer. By staying up-to-date with the latest advancements and research in prostate cancer diagnosis, clinicians can improve patient outcomes and quality of life.
Furthermore, it is essential to recognize the importance of early detection and screening in reducing mortality rates and improving treatment efficacy. As research continues to evolve, it is likely that new diagnostic techniques and biomarkers will emerge, offering even greater accuracy and precision in prostate cancer diagnosis.
Ultimately, a collaborative approach between healthcare professionals, researchers, and patients is necessary to advance our understanding of prostate cancer and improve diagnostic and therapeutic strategies, ultimately leading to better patient outcomes and improved quality of life.
This article effectively conveys complex medical concepts in an approachable manner, making it an excellent resource for patients seeking information on prostate cancer diagnosis.
This article provides a comprehensive introduction to prostate cancer diagnosis, highlighting the importance of early detection and screening methods. The language used is clear and concise, making it accessible to a wide range of readers.
While this article provides a solid overview of initial screening methods, I believe it would be strengthened by including more information on emerging diagnostic technologies or innovative approaches being explored in prostate cancer research.
The section on digital rectal exams (DREs) is informative, but could benefit from additional details on how clinicians interpret DRE findings and determine when further testing is needed.
This article does an excellent job outlining the benefits of regular screening for prostate cancer diagnosis. I particularly appreciated the discussion on how early intervention improves treatment outcomes.
As a healthcare provider, I found this article
I appreciate how this article emphasizes the significance of a thorough medical history in informing screening test selection. However, I would have liked to see more specific examples or case studies illustrating this point.