Pubic Lump Caused by STI? Know the Key
A pubic lump can be a distressing symptom, potentially indicating a sexually transmitted infection (STI). Understanding the causes and characteristics of pubic lumps is essential for prompt diagnosis and treatment.
Introduction
A pubic lump can be a concerning and potentially embarrassing symptom for individuals, particularly if they suspect it may be related to a sexually transmitted infection (STI). Recognizing the causes and characteristics of pubic lumps is crucial for prompt diagnosis and treatment, as well as preventing further transmission of potential STIs.
STIs are a significant public health concern, affecting millions of people worldwide. In addition to pubic lumps, STIs can cause a range of symptoms, including genital ulcers, discharge, and pain. However, many STIs are asymptomatic, making regular testing and screening essential for early detection and treatment.
This article aims to provide an overview of the common causes of pubic lumps, including STIs such as genital warts, herpes simplex, and chlamydia. By understanding the causes and symptoms of pubic lumps, individuals can take proactive steps to protect their health and seek medical attention if necessary.
Common Causes of Pubic Lumps
Certain STIs, such as genital warts, herpes simplex, chlamydia, and gonorrhea, can cause pubic lumps. These conditions require prompt medical attention to prevent complications and transmission to others.
Genital Warts
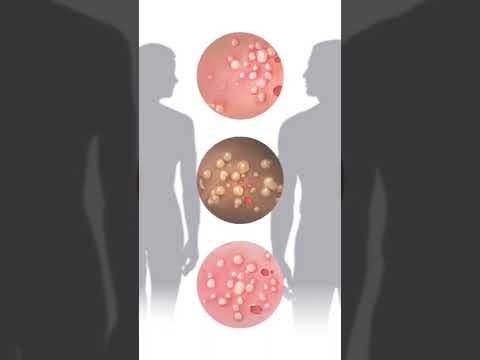
Genital warts are a common cause of pubic lumps, resulting from infection with the human papillomavirus (HPV). They typically appear as small, flesh-colored or pink growths on the vulva, vagina, cervix, penis, scrotum, or anus. Genital warts can be itchy, painful, or bleeding, and may be accompanied by discharge or odor.
HPV is highly contagious and can be spread through skin-to-skin contact during vaginal, anal, or oral sex. Genital warts can also be transmitted from mother to child during childbirth. If left untreated, genital warts can lead to serious health complications, including cervical cancer in women and penile cancer in men.
Diagnosis of genital warts typically involves a physical examination and, in some cases, biopsy or HPV DNA testing. Treatment options include cryotherapy, laser therapy, and prescription medications. Practicing safe sex, getting vaccinated against HPV, and maintaining good genital hygiene can help prevent genital warts.
Herpes Simplex
Herpes simplex virus (HSV) is another common cause of pubic lumps, particularly genital herpes. HSV-2 is primarily responsible for genital herpes, although HSV-1 can also cause genital lesions. The virus is highly contagious and can be spread through skin-to-skin contact, even when the infected individual is asymptomatic.
Genital herpes symptoms typically begin with itching, tingling, or burning sensations in the genital area, followed by the appearance of small, painful blisters or ulcers. These lesions can crust over and heal within 2-4 weeks, but the virus remains dormant and can reactivate periodically.
Diagnosis of genital herpes typically involves laboratory testing, such as PCR or viral culture. Antiviral medications can manage symptoms, reduce transmission risk, and decrease recurrence frequency. However, there is no cure for herpes simplex, emphasizing the importance of practicing safe sex and disclosing infection status to partners.
Chlamydia and Gonorrhea
Chlamydia and gonorrhea are two prevalent bacterial STIs that can cause pubic lumps, particularly in the form of lymphadenopathy or abscesses. Chlamydia trachomatis and Neisseria gonorrhoeae are the causative agents, respectively. Both infections can be asymptomatic, but symptoms may include abnormal discharge, painful urination, and genital pain.
In some cases, chlamydia and gonorrhea can cause lymph nodes in the groin area to become inflamed, leading to painful swelling. Untreated, these infections can progress to more severe complications, such as pelvic inflammatory disease (PID) in women or epididymitis in men.
Diagnosis typically involves nucleic acid amplification tests (NAATs) or cultures. Antibiotic treatment is effective against both chlamydia and gonorrhea, but antibiotic resistance is a growing concern. It is essential to complete the full treatment course and for partners to undergo testing and treatment to prevent reinfection and transmission to others.
Other Possible Causes
Beyond common STIs, other conditions can cause pubic lumps, including skin conditions, allergic reactions, and non-sexually transmitted infections. A comprehensive diagnosis is crucial to determine the underlying cause and guide effective treatment.
Syphilis
Syphilis, a bacterial infection, can cause pubic lumps, typically in the form of firm, painless chancre sores during the primary stage. If left untreated, syphilis progresses to secondary syphilis, characterized by a rash, often appearing on the palms and soles, accompanied by fever, headache, and fatigue. Tertiary syphilis can lead to serious complications, including neurological and cardiovascular problems.
A syphilis diagnosis involves blood tests and physical examination. Antibiotic treatment, usually penicillin, effectively cures syphilis. However, early detection is critical to prevent long-term damage and transmission to others. Pregnant women with syphilis can pass the infection to their unborn child, emphasizing the need for timely diagnosis and treatment.
Individuals with syphilis may not exhibit noticeable symptoms, making regular STI testing essential for those at risk. Syphilis can increase the risk of HIV transmission, underscoring the importance of comprehensive STI testing and safe sex practices.
Bacterial Vaginosis and Yeast Infections
Bacterial vaginosis (BV) and yeast infections are common vaginal conditions that can cause pubic lumps, although they are not typically classified as STIs. BV results from an imbalance of natural vaginal bacteria, while yeast infections are caused by an overgrowth of Candida fungus.
Symptoms of BV include abnormal vaginal discharge, odor, and itching, whereas yeast infections are characterized by itching, burning, and a thick, white discharge. Both conditions can cause pubic lumps, particularly if the infection spreads to the vulva or labia.
Diagnosis involves pelvic examination and laboratory tests. Treatment for BV typically involves antibiotics, while yeast infections are treated with antifungal medications. Practicing good hygiene, wearing breathable clothing, and avoiding scented products can help prevent these conditions. It is essential to seek medical attention if symptoms persist or worsen to prevent complications and promote effective treatment.
Recognizing Genital Herpes Symptoms
Genital herpes symptoms can be subtle, making timely diagnosis challenging. Understanding the characteristic signs and symptoms is crucial for prompt treatment and prevention of transmission to others, mitigating the risk of complications.
Common Symptoms
Common symptoms of genital herpes include the appearance of small, painful blisters or ulcers on the genitals, buttocks, or thighs. These lesions may crust over and heal within 2-4 weeks, only to recur in the future. Other frequent symptoms include itching, burning, or tingling sensations in the affected area, as well as swelling of the lymph nodes in the groin. Some individuals may also experience flu-like symptoms, such as fever, headache, and fatigue, particularly during the initial outbreak. Women may exhibit additional symptoms, including abnormal vaginal discharge, painful urination, and cervicitis. It is essential to note that some individuals may be asymptomatic, making regular testing and screening crucial for diagnosis and prevention of transmission.
In both men and women, the symptoms may vary in severity and frequency, and can be influenced by factors such as stress, hormonal changes, and overall health status. A thorough medical evaluation is necessary to determine the presence and severity of genital herpes.
Less Common Symptoms
In rare cases, genital herpes can also cause meningitis, an inflammation of the membranes surrounding the brain and spinal cord. This can manifest as fever, headache, stiff neck, and altered mental status. Moreover, genital herpes can increase the risk of acquiring other STIs, including HIV. It is crucial to seek medical attention if experiencing any unusual or severe symptoms, as prompt treatment can help mitigate complications and improve outcomes.
Early recognition and management of these less common symptoms are vital to preventing long-term sequelae and improving quality of life.
Importance of STI Testing
Regular STI testing is crucial for promptly diagnosing and treating infections, preventing long-term complications, and reducing transmission to others. Early detection enables effective management and improves overall health outcomes.
Why Get Tested?
Getting tested for STIs is essential for several reasons. Firstly, many STIs are asymptomatic, meaning they do not exhibit noticeable symptoms, making it difficult to diagnose without testing. Secondly, untreated STIs can lead to severe health complications, such as infertility, organ damage, and increased risk of HIV transmission. Thirdly, STIs can be transmitted to others, even if symptoms are not present, highlighting the importance of testing for prevention. Additionally, some STIs, like chlamydia and gonorrhea, can cause irreversible damage if left untreated, emphasizing the need for prompt diagnosis and treatment. Furthermore, STI testing provides an opportunity for individuals to take control of their health, make informed decisions about their relationships, and prevent the spread of infections to others. By getting tested, individuals can ensure their health and well-being, as well as that of their partners.
When to Get Tested
It is recommended to get tested for STIs regularly, especially if an individual is sexually active. Specifically, testing is advised after engaging in unprotected sex, experiencing symptoms of an STI, or having a partner diagnosed with an STI. Additionally, individuals with multiple sex partners, those who have recently changed partners, or those who have engaged in high-risk behavior, such as sharing needles, should consider regular testing; Women should also be tested during pregnancy, as some STIs can affect fetal development. The Centers for Disease Control and Prevention (CDC) recommends that all sexually active individuals aged 13-64 be tested for HIV at least once. Regular STI testing is crucial for maintaining good health, preventing the spread of infections, and ensuring timely treatment if necessary. By prioritizing testing, individuals can protect themselves and their partners from potential health risks.
In conclusion, recognizing the potential causes of a pubic lump, understanding genital herpes symptoms, and prioritizing STI testing are essential steps in maintaining reproductive health and preventing the spread of infections.
Key Takeaways
The key takeaways from this discussion on pubic lumps caused by STIs are crucial for individuals to understand and prioritize their reproductive health. Firstly, it is essential to recognize that pubic lumps can be a symptom of various STIs, including genital warts, herpes simplex, and syphilis. Secondly, early diagnosis and treatment are vital in preventing long-term complications and the spread of infections. Thirdly, STI testing should be a priority for individuals who are sexually active, especially if they have multiple partners or engage in high-risk behaviors. Lastly, awareness and education are critical in reducing the stigma associated with STIs and promoting a culture of prevention and responsibility. By taking these key takeaways into consideration, individuals can take proactive steps in maintaining their reproductive health and preventing the spread of STIs.
- Prompt diagnosis and treatment are crucial in preventing long-term complications.
- STI testing should be a priority for sexually active individuals.
Final Thoughts
In conclusion, it is imperative that individuals prioritize their reproductive health and take proactive steps in preventing the spread of STIs. By understanding the causes and symptoms of pubic lumps, individuals can seek prompt medical attention and receive effective treatment. Furthermore, it is essential to recognize that STIs are a public health concern that requires a comprehensive approach, including education, awareness, and access to healthcare services.
Healthcare providers play a critical role in promoting STI awareness and providing non-judgmental care to individuals who may be at risk of infection. By working together, we can reduce the stigma associated with STIs and promote a culture of prevention and responsibility. Ultimately, it is our collective responsibility to prioritize our health and well-being, and to take proactive steps in preventing the spread of STIs.
By doing so, we can create a healthier and more informed community, where individuals feel empowered to take control of their reproductive health.
As a healthcare professional myself , I found this article to be accurate but slightly lacking in terms specificity regarding diagnostic procedures for each condition mentioned.
I appreciate how this article emphasizes the importance of regular testing and screening for STIs. This is especially crucial for asymptomatic cases where individuals may not even know they have an infection.
The section on genital warts was particularly informative. I didn
This article provides a comprehensive overview of the common causes of pubic lumps, including STIs such as genital warts and herpes simplex. The language is clear and concise, making it accessible to a wide range of readers.
What struck me most about this piece was its ability balance sensitivity with factual presentation given subject matter often stigmatized societal discourse Well done author
One area for improvement could be providing more information on prevention methods beyond just mentioning regular testing. Perhaps discussing safe sex practices or vaccination options would add depth to the article.
While overall well-written certain sentences felt repetitive reiterating same points multiple times minor editing suggested reduce redundancy otherwise excellent resource those seeking info topic.