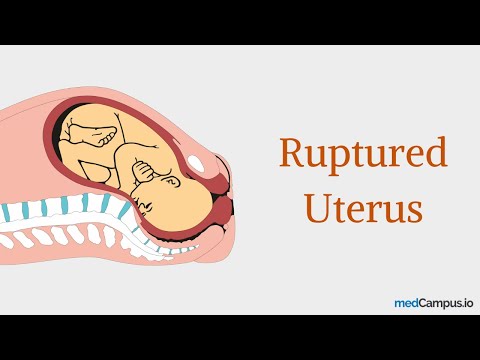
Introduction to Uterine Rupture
Uterine rupture is a life-threatening condition occurring when the uterus tears, often due to previous uterine surgery, obstetric complications, or congenital anomalies. Prompt recognition and treatment are crucial to prevent maternal and fetal morbidity and mortality.
Causes of Uterine Rupture
Uterine rupture can occur due to various factors, including⁚
- Trauma⁚ Severe abdominal trauma, such as from a car accident or fall, can cause the uterus to rupture.
- Previous uterine surgery⁚ Women who have had a previous cesarean section, hysterectomy, or other uterine surgery are at increased risk of uterine rupture.
- Congenital anomalies⁚ Women born with uterine anomalies, such as a unicornuate uterus, are at higher risk of uterine rupture.
- Obstetric complications⁚ Complications during pregnancy, such as placental abruption or multiple gestations, can increase the risk of uterine rupture.
- Uterine defects⁚ Women with pre-existing uterine defects, such as a uterine fibroid or adenomyosis, are at increased risk of uterine rupture.
It is essential to note that uterine rupture can occur without any identifiable risk factors, emphasizing the importance of close monitoring during pregnancy and prompt recognition of symptoms.
Pregnancy Complications and Uterine Defects
Pregnancy complications and uterine defects can significantly increase the risk of uterine rupture. Some common complications and defects that may contribute to uterine rupture include⁚
- Placental abruption⁚ A condition where the placenta separates from the uterus, which can cause bleeding and increase the risk of uterine rupture.
- Multiple gestations⁚ Carrying twins or other multiples can increase the risk of uterine rupture due to the increased strain on the uterus.
- Uterine fibroids⁚ Benign growths in the uterus that can weaken the uterine wall and increase the risk of rupture.
- Adenomyosis⁚ A condition where tissue similar to the lining of the uterus grows into the uterine wall, which can weaken the uterus and increase the risk of rupture.
Women with a history of pregnancy complications or uterine defects should be closely monitored during pregnancy to reduce the risk of uterine rupture. Regular prenatal care and prompt recognition of symptoms are essential in preventing adverse outcomes.
Pregnancy-Induced Uterine Rupture
Pregnancy-induced uterine rupture is a rare but life-threatening condition, often occurring in women with no prior uterine surgery or known defects. Spontaneous rupture can be caused by inherent uterine weakness or abnormal labor progression.
Symptoms of Uterine Rupture
Uterine rupture symptoms can vary in severity and may be nonspecific, making prompt diagnosis challenging. Common signs include sudden onset of severe abdominal pain, often accompanied by tenderness and guarding. The pain may radiate to the back or chest and worsen over time.
Additional symptoms may include vaginal bleeding, which can range from light spotting to severe hemorrhage, and abnormal fetal heart rate patterns. In some cases, uterine rupture may cause a decrease in fetal movement or a sudden change in the baby’s position.
Women experiencing uterine rupture may also exhibit signs of shock, such as tachycardia, hypotension, and decreased urine output. It is essential to seek immediate medical attention if any of these symptoms occur during pregnancy, as timely intervention can significantly improve outcomes for both the mother and the baby.
A high index of suspicion is crucial in diagnosing uterine rupture, as delays in recognition and treatment can result in catastrophic consequences. Healthcare providers must be vigilant in monitoring pregnant women for potential signs of uterine rupture, particularly those with a history of uterine surgery or complications.
Abdominal Pain During Pregnancy
Abdominal pain during pregnancy is a common symptom that can be caused by various factors, including uterine rupture. Women experiencing uterine rupture often report sudden, severe, and unrelenting abdominal pain that worsens over time. The pain may be localized to the lower abdomen or radiate to the back, chest, or shoulders.
The character of the pain can vary, but it is often described as sharp, stabbing, or tearing. Some women may experience a band-like sensation around their abdomen or a feeling of intense pressure. The pain may be exacerbated by movement, coughing, or deep breathing.
In some cases, abdominal pain may be accompanied by nausea, vomiting, or fever. Women with a history of uterine surgery, previous uterine rupture, or obstetric complications are at increased risk of experiencing abdominal pain due to uterine rupture. It is essential for healthcare providers to evaluate any reports of abdominal pain during pregnancy promptly and thoroughly to rule out uterine rupture and other potential causes.
A thorough physical examination, medical history, and diagnostic testing can help determine the cause of abdominal pain and guide appropriate management. Any concerns about abdominal pain during pregnancy should be addressed immediately to ensure the well-being of both the mother and the baby.
Vaginal Bleeding and Fetal Distress Signs
Vaginal bleeding, decreased fetal movement, and abnormal heart rate patterns can indicate fetal distress due to uterine rupture. Prompt recognition of these signs is crucial to initiate emergency interventions and prevent adverse outcomes for both mother and baby.
Treatments for Uterine Rupture
Immediate medical attention is essential in treating uterine rupture. The primary goal is to ensure the well-being of both the mother and the baby. Treatment options are typically surgical and may involve a multidisciplinary team of specialists.
In most cases, an emergency cesarean section is necessary to deliver the baby promptly. This procedure allows the medical team to assess the situation and manage any potential complications.
Following delivery, the extent of the uterine damage will determine the next course of action. In some instances, the uterus can be repaired, while in more severe cases, a hysterectomy may be necessary.
The decision to repair or remove the uterus depends on various factors, including the severity of the rupture, the overall health of the mother, and her reproductive goals. A thorough evaluation by the medical team will help determine the most suitable approach.
Effective management of uterine rupture requires prompt recognition, swift intervention, and a comprehensive treatment plan. By prioritizing maternal and fetal well-being, healthcare providers can optimize outcomes in these high-risk situations.
Emergency Delivery Procedures
In the event of a uterine rupture, an emergency delivery is often necessary to ensure the safety of both the mother and the baby. This typically involves an immediate cesarean section.
The procedure is usually performed under general anesthesia to minimize pain and discomfort. The surgical team will make an incision in the abdomen and uterus to deliver the baby as quickly as possible.
During the procedure, the medical team will closely monitor the baby’s heart rate and overall well-being. In some cases, additional interventions may be necessary to support the baby’s health.
Once the baby is delivered, the medical team will assess the extent of the uterine damage and determine the best course of action for repair. The primary goal is to control bleeding and stabilize the mother’s condition.
Emergency delivery procedures in cases of uterine rupture require swift and precise action. A well-coordinated response from the medical team can significantly improve outcomes for both the mother and the baby.
The rapid execution of emergency delivery procedures is crucial in preventing long-term complications and improving survival rates in cases of uterine rupture.
Repairing the Uterine Tear
Surgical repair of the uterine tear is performed by reapproximating the torn edges and reinforcing the uterus with sutures or other materials. The goal is to restore uterine integrity, control bleeding, and prevent further complications.
Prevention and Risk Reduction
Preventing uterine rupture requires careful assessment of individual risk factors and implementation of appropriate measures. Women with a history of uterine surgery or previous uterine rupture should be closely monitored throughout their pregnancy.
A thorough prenatal evaluation can help identify potential risks, allowing for timely interventions and close surveillance. Women with suspected uterine anomalies or defects may benefit from specialized imaging studies to confirm the diagnosis.
In addition to close monitoring, women at high risk for uterine rupture may be advised to have an elective cesarean delivery prior to the onset of labor. This approach can significantly reduce the risk of uterine rupture and its associated complications.
It is essential for healthcare providers to educate patients about the signs and symptoms of uterine rupture, emphasizing the importance of prompt medical attention if any concerns arise. By combining vigilant monitoring, patient education, and timely interventions, the risk of uterine rupture can be minimized, ensuring a safer pregnancy outcome.
Understanding Cesarean Section Risks
A cesarean section is a common delivery method for women with a history of uterine surgery or previous uterine rupture. However, it is essential to acknowledge the associated risks and complications.
A primary concern is the potential for placenta accreta, a condition where the placenta adheres too deeply to the uterine wall. This can lead to severe bleeding, requiring blood transfusions and potentially life-threatening interventions.
Additionally, multiple cesarean sections increase the risk of developing adhesions and scar tissue, which can lead to bowel obstruction, chronic pain, and infertility. Women undergoing repeat cesarean sections are also at a higher risk for surgical complications, such as bladder and bowel injuries.
It is crucial for healthcare providers to discuss these risks with patients, taking into account individual circumstances and medical histories. A thorough understanding of the potential complications associated with cesarean sections enables women to make informed decisions about their reproductive health and delivery options.
Monitoring for Uterine Rupture Symptoms
Close monitoring by healthcare providers is crucial for high-risk patients. Regular check-ups, fetal heart rate monitoring, and prompt reporting of symptoms can facilitate timely interventions and improve maternal and fetal outcomes in cases of uterine rupture.
In conclusion, uterine rupture is a serious and potentially life-threatening condition that requires prompt recognition and treatment. Healthcare providers must be aware of the signs and symptoms, as well as the risk factors associated with uterine rupture.
A multidisciplinary approach to care, involving obstetricians, neonatologists, and other specialists, is essential for optimal maternal and fetal outcomes. Furthermore, educating patients about the risks and warning signs of uterine rupture can empower them to seek medical attention in a timely manner.
While uterine rupture is a rare event, its impact can be significant. Ongoing research and education are necessary to improve our understanding of this condition and to develop effective strategies for prevention and treatment. Ultimately, a comprehensive approach to care can help minimize the risks associated with uterine rupture and ensure the best possible outcomes for mothers and their babies.
This article provides a comprehensive overview of uterine rupture, including its causes, risk factors, and potential complications during pregnancy. I appreciate how it emphasizes prompt recognition and treatment.
The content effectively tackles complex topics yet remains accessible.Clearly defining medical terms could make it even easier for non-medical readers.
A well-written article highlighting crucial information about uterine rupture.I would like to see further discussion on management strategies for women with previous uteriner surgery.
This piece effectively underscores critical aspects surrounding this potentially catastrophic event.I feel it might benefit from an exploration into post-traumatic stress support following an episode.
.Overall solid work discussing key concerns associated wthuterinerupture.To better inform patients perhaps future piecescan discuss emerging researchor novel therapeutic interventions.
I found this article informative but somewhat lacking in detail regarding diagnostic approaches for identifying potential risks.I would appreciate additional information on imaging techniques used.