Understanding Folliculitis
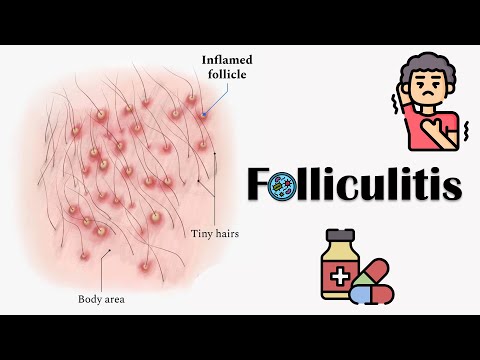
Folliculitis is a prevalent skin condition characterized by inflammation of the hair follicles, often caused by bacterial or fungal infections, resulting in skin bumps, redness, and itching, necessitating prompt attention and effective management.
Definition and Causes
Folliculitis is a skin condition defined as inflammation of the hair follicles, typically resulting from bacterial or fungal infections. The most common causes include Staphylococcus aureus bacteria, Pseudomonas aeruginosa, and fungal pathogens such as Malassezia. Other contributing factors may involve⁚
- Ingrown hairs or razor burn
- Clogged pores and excessive oil production
- Sweat and humidity
- Irritation from tight clothing or shaving
- Underlying medical conditions, such as diabetes or immunosuppression
When these factors compromise the integrity of the hair follicle, they create an ideal environment for pathogens to thrive, leading to folliculitis. Understanding the underlying causes is essential for effective prevention and treatment strategies.
A comprehensive approach to addressing these causes can help mitigate the risk of developing folliculitis and promote overall skin health.
Symptoms of Folliculitis
The clinical presentation of folliculitis typically includes small, inflamed bumps or pustules around hair follicles, accompanied by redness, itching, and tenderness, which can progress to more severe manifestations if left untreated or mismanaged.
Identifying the Signs
Accurate identification of folliculitis signs is crucial for timely intervention and effective management. Characteristic signs include small, raised, and inflamed bumps or pustules surrounding hair follicles, often accompanied by erythema, pruritus, and tenderness. In more severe cases, lesions may become larger, more painful, and suppurative. Folliculitis may be acute or chronic, with variable severity and distribution. A thorough medical history, physical examination, and diagnostic tests, such as bacterial cultures or skin scrapings, may be necessary to confirm the diagnosis and determine the underlying cause. Practitioners should remain vigilant for potential complications, including abscess formation, cellulitis, and scarring. A comprehensive understanding of folliculitis signs and symptoms enables healthcare providers to develop targeted treatment strategies, reduce morbidity, and improve patient outcomes.
- Small, raised, and inflamed bumps or pustules surrounding hair follicles
- Erythema, pruritus, and tenderness
- Lesions may become larger, more painful, and suppurative in severe cases
Early recognition and treatment of folliculitis signs can significantly impact disease progression and patient quality of life;
Folliculitis vs. Acne
Distinguishing between folliculitis and acne is essential for accurate diagnosis and effective treatment. While both conditions present with skin lesions and inflammation, they exhibit distinct characteristics. Folliculitis typically involves the hair follicle, with lesions centered around the follicular opening, whereas acne primarily affects the sebaceous gland. The morphology of lesions also differs, with folliculitis often presenting with small, pus-filled pustules, and acne characterized by comedones, papules, and pustules. Furthermore, the distribution of lesions varies, with folliculitis commonly affecting areas with thick or curly hair, such as the beard, scalp, or groin, and acne typically occurring on the face, chest, and back. A thorough clinical evaluation, including a detailed medical history and physical examination, is necessary to differentiate between these two conditions and develop an appropriate treatment plan.
- Folliculitis involves the hair follicle, while acne affects the sebaceous gland
- Lesion morphology and distribution differ between the two conditions
- Accurate diagnosis is crucial for effective treatment and management
Types of Folliculitis
Folliculitis can be broadly categorized into bacterial, fungal, viral, and non-infectious types, each with distinct etiologies and clinical presentations, requiring tailored approaches to diagnosis, treatment, and management.
Bacterial Folliculitis
Bacterial folliculitis is a type of folliculitis caused by bacterial infections, typically Staphylococcus aureus. It is characterized by the formation of pus-filled pimples or pustules around the hair follicles, often accompanied by redness, swelling, and itching.
This type of folliculitis can occur anywhere on the body, but it is most common on the face, arms, legs, and buttocks. Bacterial folliculitis can be superficial or deep, with the latter being more severe and potentially leading to scarring.
Risk factors for developing bacterial folliculitis include poor hygiene, shaving or waxing, using hot tubs or whirlpools, and having underlying medical conditions such as diabetes or obesity. Prompt treatment with antibiotics is essential to prevent further complications and promote healing.
In addition to antibiotics, warm compresses and good wound care can help manage symptoms and promote recovery. In severe cases, bacterial folliculitis may require drainage of infected lesions or other surgical interventions.
Fungal Folliculitis
Fungal folliculitis, also known as Malassezia folliculitis, is a type of folliculitis caused by fungal infections, typically Malassezia species. It is characterized by the formation of itchy, inflamed papules and pustules around the hair follicles, often on the chest, back, and shoulders.
This type of folliculitis thrives in warm, humid environments and is more common in individuals with oily skin or those who engage in activities that cause excessive sweating. Fungal folliculitis can also be triggered by certain medications, such as corticosteroids and antibiotics.
Diagnosis of fungal folliculitis involves microscopic examination of skin scrapings or biopsy samples. Treatment typically involves antifungal medications, either topical or oral, depending on the severity of the condition. Good hygiene practices, such as regular showering and wearing loose-fitting clothing, can also help manage symptoms and prevent recurrence.
In some cases, fungal folliculitis may require ongoing maintenance therapy to prevent relapse. It is essential to consult a healthcare professional for proper diagnosis and treatment to ensure effective management of this condition.
Folliculitis Treatment
Effective folliculitis treatment involves a multifaceted approach, incorporating home remedies, medical treatments, and lifestyle modifications to alleviate symptoms, eliminate underlying causes, and prevent recurrence, ensuring optimal outcomes for affected individuals.
Home Remedies
Several home remedies can provide relief from folliculitis symptoms. Applying a warm compress to the affected area can help reduce inflammation and promote drainage. A mixture of equal parts water and white vinegar can be used as a topical treatment to balance the skin’s pH and combat bacterial growth.
- Tea tree oil, known for its antimicrobial properties, can be applied topically to combat infection-causing microorganisms.
- Aloe vera gel can be used to soothe and calm irritated skin, reducing redness and itching.
- Exfoliating gentle scrubs containing sugar or salt can help remove dead skin cells and unclog pores.
It is essential to note that while home remedies can provide relief, they may not address the underlying cause of folliculitis. If symptoms persist or worsen, it is crucial to consult a healthcare professional for further guidance and treatment.
Additionally, maintaining good hygiene practices, such as regularly washing the affected area with mild soap and lukewarm water, can help prevent the spread of infection and promote healing.
Medical Treatments
For more severe cases of folliculitis, medical treatments may be necessary to effectively manage symptoms and address the underlying cause of the condition.
Topical antibiotics, such as erythromycin or clindamycin, may be prescribed to treat bacterial folliculitis, while antifungal medications, like ketoconazole, may be used to combat fungal infections.
In some cases, oral antibiotics or antifungals may be necessary to treat more widespread or severe infections.
- Corticosteroid creams or ointments can be used to reduce inflammation and swelling.
- Retinoid creams or gels may be prescribed to help prevent clogged pores and reduce the risk of future breakouts.
It is essential to follow a healthcare professional’s instructions and complete the full course of treatment to ensure effective management of folliculitis and prevent recurrence.
In addition to these treatments, a healthcare professional may also recommend lifestyle modifications, such as avoiding tight clothing and shaving, to help alleviate symptoms and promote healing.
Preventing Folliculitis
Effective prevention strategies involve adopting good hygiene practices, using gentle skin care products, and avoiding irritants, ultimately reducing the risk of folliculitis and promoting overall skin health and well-being.
Skin Care Tips
To prevent folliculitis, it is essential to maintain good skin hygiene. Wash the affected area with a mild soap and lukewarm water, twice a day. Avoid using harsh or abrasive cleansers, as they can strip the skin of its natural oils and cause irritation.
Exfoliating regularly can help remove dead skin cells and prevent clogged pores. However, be gentle and avoid over-exfoliating, as this can lead to further irritation. Additionally, shaving and waxing can cause micro-tears in the skin, making it more susceptible to infection.
Using a non-comedogenic moisturizer can help keep the skin hydrated and balanced. Avoid sharing personal care items, such as towels or razors, to prevent the spread of infection. By following these simple skin care tips, individuals can significantly reduce their risk of developing folliculitis and maintain healthy, clear skin.
It is also crucial to avoid tight clothing and tight hairstyles that can cause friction and lead to folliculitis. Keeping the skin clean and dry, especially after exercising or sweating, can also help prevent the development of folliculitis.
Avoiding Irritants
To prevent folliculitis, it is crucial to identify and avoid potential irritants that can cause skin inflammation and infection; Common irritants include harsh chemicals, such as those found in cleaning products, pesticides, and heavy metals.
Tight clothing made from synthetic fabrics, such as nylon or polyester, can also cause friction and irritation, increasing the risk of folliculitis. Additionally, certain makeup and skincare products can clog pores and cause skin irritation, making it essential to choose products labeled “non-comedogenic” or “hypoallergenic.”
Exposure to extreme temperatures, such as those experienced in saunas or hot tubs, can also cause skin irritation and increase the risk of folliculitis. Furthermore, avoiding activities that cause excessive sweating, such as intense exercise or physical labor, can help reduce the risk of folliculitis. By being aware of and avoiding these potential irritants, individuals can significantly reduce their risk of developing folliculitis.
Avoiding sharing personal items, such as towels or razors, and using clean equipment when engaging in activities like shaving or waxing, can also help prevent the spread of infection and reduce the risk of folliculitis.
In conclusion, understanding folliculitis is crucial for effective management and prevention, and by being aware of its causes, symptoms, and treatment options, individuals can take proactive steps to maintain healthy skin and overall well-being.
Importance of Awareness
Raising awareness about folliculitis is essential to promote early detection, proper treatment, and prevention. By educating individuals about the causes, symptoms, and management strategies, they can take control of their skin health and adopt habits that reduce the risk of developing this condition. Awareness also helps to dispel misconceptions and stigmas associated with skin conditions, encouraging individuals to seek medical attention without hesitation. Furthermore, awareness campaigns can promote research and development of more effective treatments, ultimately improving the quality of life for those affected by folliculitis. Healthcare professionals, educators, and individuals must work together to spread awareness and promote a culture of skin health, enabling people to make informed decisions about their well-being and seek timely medical attention if symptoms arise.
This article provides an excellent overview of folliculitis, covering its definition, causes, symptoms, and importance of prompt attention. The writing style is clear and concise.
I found this article very informative about the underlying causes of folliculitis. The section on ingrown hairs was particularly helpful for me.
As a dermatologist, I appreciate the accuracy of this article in discussing the pathophysiology of folliculitis. However, I would have liked to see more emphasis on evidence-based treatments.
While this article provides a solid foundation on understanding folliculitis symptoms might consider expanding upon differential diagnoses.
The writing style was engaging but could benefit from additional visuals to illustrate key points about skin anatomy.
This article effectively highlights the importance of proper hygiene practices in preventing folliculitis.