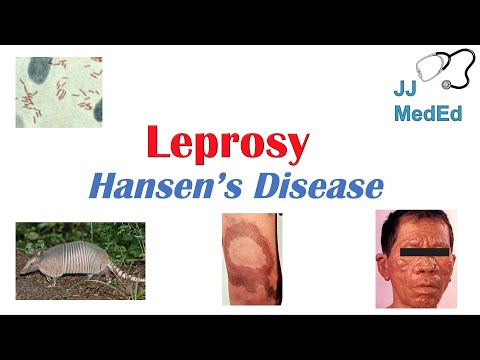
Introduction to Leprosy Disease
Leprosy, also known as Hansen’s disease, is a chronic bacterial infection affecting the nerves, skin, and mucous membranes. It is one of the oldest recorded contagious diseases, with a rich history and varied global prevalence.
Causes and Transmission of Leprosy
Leprosy is caused by Mycobacterium leprae bacteria, primarily transmitted through respiratory droplets from infected individuals, with a long incubation period, typically 3-5 years٫ before symptoms manifest٫ allowing for silent transmission.
Bacterial Infection
Leprosy is caused by the bacterium Mycobacterium leprae, a slow-growing, acid-fast bacillus that primarily infects the skin, peripheral nerves, and mucous membranes. The bacteria have a unique tropism for cooler body regions, such as the skin and peripheral nerves, which is why leprosy manifestations often occur in these areas.
The bacterial infection leads to an immune response, which can be divided into two main categories⁚ tuberculoid and lepromatous leprosy. Tuberculoid leprosy is characterized by a strong cellular immune response, while lepromatous leprosy is marked by a poor cellular immune response, leading to widespread bacterial dissemination.
Understanding the bacterial infection and its interaction with the host immune system is crucial for developing effective diagnostic and therapeutic strategies against leprosy. Research has made significant progress in elucidating the pathogenesis of M. leprae infection, but further studies are needed to fully comprehend the mechanisms underlying this complex disease.
Armadillos as an Infection Source
In addition to human-to-human transmission, leprosy can also be acquired through contact with infected armadillos. The nine-banded armadillo (Dasypus novemcinctus) is a natural reservoir for Mycobacterium leprae, and handling or consuming undercooked meat from infected animals can lead to infection.
Studies have shown that armadillos can harbor large numbers of M. leprae bacteria, which can be shed into the environment through their saliva, urine, and feces. This shedding can contaminate soil, water, and other environmental surfaces, posing a risk to humans who come into contact with these contaminated areas.
People who engage in activities such as hunting, cooking, or handling armadillos are at increased risk of acquiring leprosy from these animals. Awareness of this risk factor is essential for preventing leprosy transmission, particularly in regions where armadillos are common and the disease is endemic.
Symptoms of Leprosy
Leprosy symptoms can vary widely, but often include skin lesions, nerve damage, and discoloration. Early detection is crucial, as untreated leprosy can lead to permanent disability and disfigurement, impacting quality of life.
Skin Lesions and Nerve Damage
Leprosy is characterized by the presence of skin lesions, which can be flat or raised, and may be lighter or darker than the surrounding skin. These lesions can be numb to the touch, and may not produce the normal sensations of pain, heat, or cold. As the disease progresses, nerve damage can occur, leading to loss of sensation in the affected areas.
Nerve damage can also cause muscle weakness, paralysis, and disability. In severe cases, leprosy can lead to claw hand, foot drop, and other deformities. The nerve damage associated with leprosy can be irreversible if left untreated, emphasizing the importance of early detection and treatment. A comprehensive examination of the skin and nerves is necessary to assess the extent of the damage and develop an effective treatment plan.
Early detection and treatment of leprosy can help prevent long-term nerve damage and disability. It is essential to seek medical attention immediately if symptoms persist or worsen over time.
Skin Discoloration and Other Symptoms
In addition to skin lesions and nerve damage, leprosy can cause a range of other symptoms, including skin discoloration. The skin may become lighter or darker in patches, and the hair may turn white or fall out. The eyes, eyebrows, and eyelashes may also be affected, leading to vision problems and sensitivity to light.
Some people with leprosy may experience a tingling sensation or numbness in the hands and feet, which can make it difficult to feel pain or temperature changes. Others may develop muscle weakness, fatigue, or swelling in the face, hands, or feet. In rare cases, leprosy can cause inflammation of the testicles, leading to infertility or erectile dysfunction.
The symptoms of leprosy can vary widely from person to person, and may progress slowly over many years. A thorough medical examination and diagnostic testing are necessary to determine the extent of the disease and develop an effective treatment plan.
Diagnosis and Treatment of Leprosy
Accurate diagnosis and timely treatment of leprosy are crucial to prevent long-term damage and disability. A comprehensive diagnostic approach and effective treatment strategies can significantly improve patient outcomes and quality of life.
Diagnosis Methods
Diagnosing leprosy involves a combination of clinical evaluation, laboratory tests, and histopathological examination. A thorough physical examination is conducted to identify characteristic skin lesions, nerve damage, and other symptoms. Skin scrapings or biopsy samples may be collected for bacteriological index assessment, which measures the bacterial load in the affected area.
In addition, serological tests can detect specific antibodies against the causative bacteria, aiding in diagnosis. Molecular techniques, such as polymerase chain reaction (PCR), may also be employed to confirm the presence of Mycobacterium leprae DNA in tissue samples. Histopathological examination of skin and nerve biopsy specimens can provide further evidence of the disease, showcasing characteristic granulomatous inflammation and nerve damage.
A skilled healthcare professional, often with expertise in dermatology or infectious diseases, should conduct the diagnostic evaluation to ensure accurate and timely diagnosis. Early detection and treatment are essential in preventing long-term consequences and improving patient outcomes.
Antibiotics Treatment and Multidrug Therapy (MDT)
The primary treatment for leprosy is multidrug therapy (MDT), a regimen consisting of two or more antibiotics that effectively target Mycobacterium leprae. The most commonly used antibiotics are rifampicin, clofazimine, and dapsone. MDT has significantly improved treatment outcomes, reducing the risk of resistance and promoting more rapid recovery.
Patients with paucibacillary leprosy typically receive a shorter treatment course, usually 6 months, whereas those with multibacillary leprosy require a 12-month regimen. It is essential to complete the full treatment course, even if symptoms appear to have resolved, to ensure the infection is fully cleared and minimize the risk of relapse or transmission to others.
Treatment with MDT has been widely adopted and is considered highly effective in curing leprosy. However, individual patient responses may vary, and careful monitoring by healthcare professionals is necessary to address any concerns or complications that may arise during treatment.
World Health Organization (WHO) Guidelines
The World Health Organization (WHO) has established comprehensive guidelines for the diagnosis, treatment, and management of leprosy. These guidelines emphasize the importance of timely detection, proper classification, and effective treatment to prevent disability and reduce transmission.
According to WHO guidelines, leprosy treatment should be provided free of charge, and patients should receive multidrug therapy (MDT) under the supervision of a healthcare professional. The guidelines also recommend regular follow-up assessments to monitor response to treatment and detect potential complications.
In addition to treatment protocols, the WHO guidelines outline strategies for controlling leprosy transmission, including contact tracing, chemoprophylaxis, and vaccination. The guidelines also emphasize the importance of integrating leprosy services into existing healthcare systems, promoting community awareness, and addressing social stigma associated with the disease.
By following WHO guidelines, healthcare providers can ensure that individuals affected by leprosy receive high-quality care, improving treatment outcomes and reducing the global burden of this disease.
Complications and Prevention
Untreated leprosy can lead to severe complications, including permanent nerve damage, disfigurement, and disability. Preventive measures, such as early detection, vaccination, and chemoprophylaxis, are crucial in reducing the risk of complications and transmission.
Preventing Complications
Preventing complications is a critical aspect of leprosy management. Early detection and treatment are essential in preventing permanent nerve damage, disfigurement, and disability. Patients with leprosy should be regularly monitored for signs of nerve damage, such as numbness, tingling, or muscle weakness. Additionally, patients should be educated on proper wound care and hygiene practices to prevent secondary infections.
Regular follow-up appointments with healthcare providers are also crucial in preventing complications. This allows for prompt identification and treatment of any emerging issues, reducing the risk of long-term damage. Furthermore, patients with leprosy should be encouraged to maintain a healthy lifestyle, including a balanced diet and regular exercise, to help prevent secondary health problems. By taking a proactive approach to prevention, individuals with leprosy can reduce their risk of complications and improve their overall quality of life.
Effective preventive measures can significantly reduce the risk of complications, enabling individuals with leprosy to lead active and productive lives.
Prevention Methods
Prevention of leprosy involves a multi-faceted approach. One key method is through vaccination, particularly the BCG vaccine, which has been shown to provide some level of protection against leprosy. Additionally, practicing good hygiene and sanitation, such as washing hands regularly, can help reduce the risk of transmission.
Avoiding close contact with individuals infected with leprosy, especially those with untreated or active infections, is also essential. Furthermore, reducing exposure to armadillos, which are known carriers of the bacteria, can also help prevent transmission. In areas where leprosy is endemic, implementing public health measures such as surveillance, screening, and education programs can help control the spread of the disease.
Early detection and treatment of leprosy cases are also critical in preventing the spread of the disease. This requires a well-functioning healthcare system and access to diagnostic and treatment services. By combining these prevention methods, it is possible to significantly reduce the incidence of leprosy and ultimately eliminate the disease.
In conclusion, leprosy is a complex and multifaceted disease that requires a comprehensive approach to prevention, diagnosis, and treatment. Despite its long history and the progress made in controlling the disease, leprosy remains a significant public health challenge in many parts of the world.
Ongoing efforts are needed to improve access to diagnostic and treatment services, particularly in resource-poor settings where the disease is most prevalent. Additionally, continued research into the causes and consequences of leprosy is essential for developing more effective prevention and treatment strategies.
By working together, healthcare providers, policymakers, and communities can help reduce the burden of leprosy and ultimately achieve a world where this ancient disease is no longer a major public health concern. This goal is ambitious, but with persistence and dedication, it is achievable. Ultimately, a future free from the suffering and stigma of leprosy is possible.
This article provides a solid foundation for understanding leprosy disease. However, I believe it would benefit from additional information on current research efforts and future directions in leprosy research.
The discussion on tuberculoid and lepromatous leprosy is clear and concise. However, I think it would be beneficial to include more details on the clinical manifestations of each type.
I appreciate how this article emphasizes the importance of early detection and treatment in preventing long-term damage from leprosy. However, I would like to see more information on access to healthcare services for individuals affected by leprosy.
Overall, this article provides a well-rounded introduction to leprosy disease. However, I think it would benefit from additional visuals or diagrams to illustrate key concepts.
I found the section on armadillos as an infection source fascinating. However, I am concerned about the potential risks of handling or consuming undercooked meat from infected animals.
I appreciate how this article highlights the importance of understanding the immune response in developing diagnostic and therapeutic strategies against leprosy. However, I would like to see more information on current treatment options.
This article provides a comprehensive overview of leprosy disease, including its causes, transmission, and bacterial infection mechanisms. The section on armadillos as an infection source is particularly informative.