Introduction
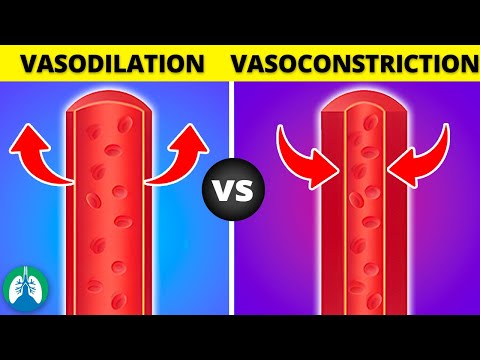
The cardiovascular system relies on precise regulation of blood flow and blood pressure to maintain homeostasis. Two critical mechanisms, vasodilation and vasoconstriction, modulate blood vessel diameter to achieve this balance. Understanding these processes is essential for comprehending cardiovascular physiology and pathophysiology.
What is Vasodilation?
Vasodilation is the process by which blood vessels increase in diameter, allowing for enhanced blood flow and reduced blood pressure. This phenomenon occurs in various vascular beds, including arteries, veins, and capillaries. Vasodilation is crucial for maintaining tissue perfusion and overall cardiovascular health.
During vasodilation, the smooth muscle cells within the blood vessel walls relax, leading to a decrease in vascular resistance. This relaxation enables the vessel to dilate, thereby increasing its cross-sectional area and allowing more blood to flow through it. As a result, the delivery of oxygen and nutrients to tissues is augmented, while the removal of waste products is also facilitated.
Vasodilation plays a pivotal role in various physiological responses, such as exercise-induced hyperemia, where increased blood flow is required to meet the heightened metabolic demands of exercising muscles. Additionally, vasodilation is essential for thermoregulation, as it enables the body to dissipate excess heat through increased blood flow to the skin’s surface.
The complex mechanisms governing vasodilation involve an interplay between various cellular and molecular components. The endothelium, a monolayer of endothelial cells lining blood vessels, plays a critical role in regulating vasodilation. Endothelial cells produce and release various signaling molecules that modulate vascular tone, such as nitric oxide, which is a potent vasodilator.
A comprehensive understanding of vasodilation is vital for elucidating the pathophysiology of various cardiovascular disorders, including hypertension, atherosclerosis, and peripheral artery disease. Furthermore, knowledge of vasodilation informs the development of therapeutic strategies aimed at improving cardiovascular health and alleviating disease-related symptoms.
Vasodilation is characterized by the relaxation of vascular smooth muscle cells, resulting in a decrease in vascular resistance and an increase in blood vessel diameter. This process is mediated by a complex interplay between various signaling molecules, ion channels, and intracellular pathways.
The primary mechanisms underlying vasodilation involve the activation of potassium channels, which lead to hyperpolarization of vascular smooth muscle cells. This hyperpolarization reduces the activity of voltage-dependent calcium channels, thereby decreasing intracellular calcium levels and promoting relaxation.
In addition, the production and release of endothelium-derived relaxing factors, such as nitric oxide, prostacyclin, and endothelium-derived hyperpolarizing factor, contribute to vasodilation. These molecules bind to specific receptors on vascular smooth muscle cells, triggering a cascade of downstream signaling events that ultimately lead to relaxation.
The mechanical properties of blood vessels also play a crucial role in vasodilation. The compliance of blood vessels, which refers to their ability to expand in response to increased pressure, enables them to accommodate increased blood flow. Furthermore, the viscoelastic properties of blood vessels influence the rate and extent of vasodilation.
Overall, the precise regulation of vasodilation involves a multifaceted interplay between cellular, molecular, and mechanical components. Understanding these mechanisms is essential for elucidating the physiological and pathological processes that govern vascular function and for developing effective therapeutic strategies to modulate vasodilation in various disease states.
Role of Nitric Oxide and Endothelium
Nitric oxide, produced by endothelial cells, plays a pivotal role in vasodilation; It stimulates guanylate cyclase, increasing cyclic GMP, which relaxes vascular smooth muscle cells. The endothelium regulates nitric oxide production, modulating vasodilation in response to various physiological and pathological stimuli.
What is Vasoconstriction?
Vasoconstriction is the decrease in diameter of blood vessels, which increases peripheral resistance and subsequently elevates blood pressure. It is a vital mechanism that counteracts vasodilation, enabling the body to redirect blood flow to areas of high demand or maintain systemic blood pressure during periods of hypotension.
The process of vasoconstriction involves the contraction of smooth muscle cells in the tunica media of arteries and arterioles. This contraction can be stimulated by various factors, including neural, hormonal, and local signals. The contraction of smooth muscle cells reduces the lumen diameter, thereby increasing vascular resistance and reducing blood flow to downstream tissues.
Vasoconstriction plays a crucial role in various physiological processes, such as maintaining blood pressure during standing, exercise, or cold exposure. It also contributes to the redistribution of blood flow during periods of stress or injury. However, excessive or inappropriate vasoconstriction can lead to pathological conditions, including hypertension, ischemia, and tissue damage; Understanding the mechanisms and regulation of vasoconstriction is essential for comprehending cardiovascular physiology and developing therapeutic strategies for related disorders.
In addition to its physiological roles, vasoconstriction has significant clinical implications. Abnormalities in vasoconstriction have been implicated in various diseases, including hypertension, atherosclerosis, and peripheral artery disease. Therefore, elucidating the mechanisms of vasoconstriction is crucial for the development of novel therapeutic approaches to treat these conditions.
Definition and Mechanism
Vasodilation is the increase in diameter of blood vessels, which reduces peripheral resistance and subsequently decreases blood pressure. This process involves the relaxation of smooth muscle cells in the tunica media of arteries and arterioles, leading to an increase in lumen diameter and a reduction in vascular resistance.
The mechanism of vasodilation involves a complex interplay between various cellular and molecular components. The process is initiated by the release of vasodilatory substances, such as nitric oxide, prostaglandins, and bradykinin, which bind to specific receptors on the surface of smooth muscle cells. This binding triggers a signaling cascade that ultimately leads to the relaxation of smooth muscle cells and the dilation of blood vessels.
The relaxation of smooth muscle cells is mediated by the activation of various signaling pathways, including the cyclic guanosine monophosphate (cGMP) pathway and the cyclic adenosine monophosphate (cAMP) pathway. These pathways converge to inhibit the contraction of smooth muscle cells, leading to a decrease in vascular tone and an increase in blood flow. The vasodilatory response is also modulated by the endothelium, which plays a crucial role in regulating vascular tone by releasing vasodilatory substances and influencing the activity of smooth muscle cells.
The vasodilatory mechanism is essential for maintaining tissue perfusion and regulating blood pressure. Abnormalities in this mechanism have been implicated in various cardiovascular diseases, including hypertension, atherosclerosis, and peripheral artery disease. Understanding the definition and mechanism of vasodilation is crucial for developing therapeutic strategies to treat these conditions.
Role of Sympathetic Nervous System
The sympathetic nervous system plays a crucial role in vasoconstriction by releasing neurotransmitters, such as norepinephrine, which stimulate alpha-adrenergic receptors on smooth muscle cells, leading to contraction and decreased blood vessel diameter, thereby increasing peripheral resistance and blood pressure.
Regulation of Vasodilation and Vasoconstriction
The regulation of vasodilation and vasoconstriction is a complex process that involves the coordinated effort of various physiological systems. The autonomic nervous system, which comprises the sympathetic and parasympathetic nervous systems, plays a crucial role in modulating blood vessel diameter.
In addition to neural control, local regulatory mechanisms also contribute to the regulation of vasodilation and vasoconstriction. These mechanisms involve the release of vasoactive substances by endothelial cells, smooth muscle cells, and other cell types. For example, the release of nitric oxide by endothelial cells can stimulate vasodilation, while the release of endothelin-1 can stimulate vasoconstriction.
Hormonal influences, such as those exerted by the renin-angiotensin-aldosterone system, also play a significant role in regulating blood vessel diameter. Furthermore, local metabolic factors, such as changes in oxygen delivery and carbon dioxide production, can also influence blood vessel diameter.
Overall, the regulation of vasodilation and vasoconstriction is a multifaceted process that involves the integration of neural, hormonal, and local regulatory mechanisms. Understanding these complex interactions is essential for appreciating the intricate mechanisms that govern cardiovascular function and for developing effective therapeutic strategies for cardiovascular disease.
Autonomic Nervous System
The autonomic nervous system (ANS) plays a pivotal role in regulating vasodilation and vasoconstriction. The ANS comprises two branches⁚ the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). These branches exert opposing effects on blood vessel diameter.
The SNS is responsible for the “fight or flight” response, which involves the release of neurotransmitters such as norepinephrine and epinephrine. These neurotransmitters stimulate the contraction of smooth muscle cells, leading to vasoconstriction. In contrast, the PNS promotes relaxation and vasodilation through the release of neurotransmitters such as acetylcholine.
The balance between SNS and PNS activity determines the net effect on blood vessel diameter. For example, during periods of stress or exercise, the SNS is activated, leading to vasoconstriction and increased blood pressure. Conversely, during periods of relaxation or sleep, the PNS is dominant, resulting in vasodilation and decreased blood pressure.
The ANS also regulates the release of hormones that influence vasodilation and vasoconstriction. For instance, the SNS stimulates the release of renin, which activates the renin-angiotensin-aldosterone system, leading to vasoconstriction. Overall, the ANS plays a critical role in modulating blood vessel diameter and maintaining cardiovascular homeostasis.
The precise regulation of the ANS is essential for maintaining optimal cardiovascular function. Dysregulation of the ANS has been implicated in various cardiovascular disorders, including hypertension and heart failure.
Local Regulation
Local factors, such as tissue oxygenation, carbon dioxide levels, and pH, also influence blood vessel diameter. For example, decreased oxygen delivery to tissues triggers vasodilation, increasing blood flow and oxygen supply. This intrinsic regulation ensures optimal perfusion of tissues and organs.
In conclusion, vasodilation and vasoconstriction are intricate mechanisms that play a crucial role in maintaining cardiovascular homeostasis. The delicate balance between these two processes ensures optimal blood flow, blood pressure, and oxygen delivery to tissues and organs.
Dysregulation of vasodilation and vasoconstriction has been implicated in various cardiovascular diseases, including hypertension, atherosclerosis, and heart failure. Therefore, understanding the complex interplay between these mechanisms is essential for the development of effective therapeutic strategies.
Further research is necessary to elucidate the molecular mechanisms underlying vasodilation and vasoconstriction, as well as to explore novel therapeutic targets for cardiovascular disease. A comprehensive understanding of these processes will ultimately contribute to the improvement of cardiovascular health and the reduction of morbidity and mortality associated with cardiovascular disease.
Moreover, the importance of vasodilation and vasoconstriction extends beyond the realm of cardiovascular physiology, as these mechanisms also play a critical role in regulating blood flow and oxygen delivery in other organ systems. As such, continued investigation into these processes will have far-reaching implications for our understanding of human physiology and pathophysiology.
Ultimately, the study of vasodilation and vasoconstriction serves as a paradigm for the complex and dynamic interplay between various physiological mechanisms, highlighting the importance of integrative research approaches in advancing our understanding of human biology.
The article highlights the significance of vasodilation in exercise-induced hyperemia and thermoregulation, providing valuable insights into its physiological applications.
I appreciated the emphasis on nitric oxide as a potent vasodilator; however, I felt that other signaling molecules were glossed over too quickly.
I found the explanation of the mechanisms governing vasodilation to be clear and concise, particularly the role of endothelial cells.
The writing style is clear and engaging, making it accessible to readers with varying levels of background knowledge.
The article effectively balances technical detail with readability; however, additional illustrations or diagrams would enhance comprehension.
While the article provides a solid foundation for understanding vasodilation, I would have liked to see more discussion on its clinical implications.
This article provides an excellent introduction to the concept of vasodilation and its importance in maintaining cardiovascular health.